3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2015; 6(2):177-183. doi:10.7150/jca.10482 This issue Cite
Research Paper
Brain and Central Nervous System Cancer Incidence in Navarre (Spain), 1973-2008 and Projections for 2014
1. Department of Statistics and O. R., Public University of Navarre, Spain.
2. Epidemiology Unit, Navarre Public Health Institute, Spain.
3. CIBER Epidemiología y Salud Pública (CIBERESP), Spain
4. Red de Investigación en Servicios de Salud en Enfermedades Crónicas (REDISSEC), Spain
Received 2014-9-4; Accepted 2014-10-15; Published 2015-1-5
Abstract
Different studies have pointed out Navarre as one of the regions of Spain with the highest incidence rates of brain and other central nervous system (CNS) cancer. Trend analysis for cancer incidence rates for long periods of time, might help determining risk factors as well as, assessing prevention actions involved in this disease. The objective of this study was to describe the incidence of brain and CNS cancer using data from the population-based cancer registry of Navarre, (Spain) during the period 1973-2008 and provide forecast figures up to-2014. Crude and age-standardized (world population) incidence rates of brain cancer per 100,000 person-years were calculated by the direct method separately by gender, area (Pamplona and others), and age-groups. Penalized splines for smoothing rates in the temporal dimensions were applied in order to estimate and forecast cancer incidence rates. Age-adjusted incidence rates showed an increase over the study and forecast periods in both sexes more marked in women than in men. Higher incidence rates were observed in men compared with women but the differences became smaller with time. The increase was due to the rise of rates in the oldest age groups since the rates for younger age groups remained stable or decreased over time. As the entire aetiology of brain and other CNS cancer is not still clear, keep promoting healthful lifestyles for cancer primary prevention among the whole population is necessary.
Keywords: Brain Cancer Incidence, Trend analysis, Projections, Population-based cancer registries, Spain
Introduction
According to the latest brain and other nervous system cancer figures published by GLOBOCAN, 139,608 and 116,605 new cases were diagnosed in 2012 worldwide in male and female, representing 3.9 and 3.0 per 100,000 person-years [1]. Data from the International Agency for Research on Cancer (IARC) publication, Cancer Incidence in Five Continents (CI5C), Vol. X (2003-2007), show high brain cancer incidence rates in Navarre, Spain: 7.8 and 5.7 per 100,000 in male and female respectively, which are among the first twelve highest rates registered for each gender [2]. Brain and nervous system cancer represents 2.3% of the total cancer incident cases registered in Navarre [2]. Navarre is one of the 17 Autonomous Regions of Spain located in the north of the country at the western end of the Pyrenees, bordering the Basque Country, La Rioja, and Aragon in Spain and Aquitaine in France.
This region has historically shown high brain cancer incidence and mortality rates. A previous geographical analysis of brain cancer mortality performed in Spain showed a cluster of highest risk for Navarre and Basque Country regions. These results shown in the Atlas of Mortality for Cancer and other Causes in Spain (1978-1992) [3] revealed high risk of brain cancer mortality in Navarre, which registered the highest rates in Spain for both sexes, with a male mortality rate of 8.45 per 100,000 person-years versus a figure of 5.44 for Spain as a whole, and a female mortality rate of 4.69 versus a national figure of 3.30. These rates were adjusted using the European standard population [4]. Those figures motivated the performance of another geographical study in Navarre and the Basque Country where the association of brain cancer incidence and the types of crop and phytosanitary treatments used in rural areas were analyzed [5]. In that study, the authors did not find association between brain cancer incidence pattern and the use of specific type of land cover and/or crop in those regions.
Regarding the causes of brain and other central nervous system (CNS) tumours, it is generally accepted that brain cancer may be due to an alteration in the person's inherited genetic factors or caused by environmental factors [6-9]. Some studies have found a positive association between brain cancer and the socioeconomic status [10-13]. In this sense, Navarre is ranked in the highest quintiles as regards per capita income among Spain's regions [14]. The use of mobile phones has also been investigated as a risk factor [16]. These researchers followed up the mobile phone subscriber since 1982-95 until 2007 in Denmark, with a focus on tumours of the CNS. The authors did not find evidence of an increased risk of tumours of the CNS. Moreover, they investigated the effects on people who had used mobile phones for 10 years or more, and this long term use was not associated with higher risks of cancer.
The aim of this study is to provide a descriptive trend analysis of population-based brain and CNS cancer incidence in Navarre, between 1973 and 2008, by gender, age-groups and by two geographical areas. The trends of morphological groups are also provided during the study period. Finally, projections of cancer incidence rates by gender and age-groups are also presented until 2014.
Material and Methods
This study is based on brain and CNS tumour incident cases (C70-C72, International Classification of Diseases-10) reported to the Navarre Cancer Registry. A detailed description of this registry is given elsewhere [2, 17, 18]. To guarantee the production of reliable data, the Navarre Cancer Registry has quality-control procedures based on the following quality indicators: the percentage of death-certificate-only registrations (DCO), the percentage of microscopically verified cases (MV), the percentage of cases for which the age was unknown (UA) and the percentage of unspecific morphology (UM). The indicators for the period 2003-2008 for this specific site were 1.0% of DCO, 53.9% of MV, 0% of UA and 13.7% of UM.
In this study, the brain and CNS cancer incident cases, codes C71-C72 according to the 10th revision of International Classification of Diseases (ICD-10) [19], diagnosed between 1973 and 2008 were included. The population size at risk by 5-year age groups and gender was acquired from the Statistical Institute of Navarre [20]. Cases coded as C71-C72 (excluding C70) were histologically classified following the morphological groups of brain and CNS cancer defined in CI5C Vol IX [21]: gliomas (9380-9384, 9371-9460), embryonal tumours (9470-9474, 9490, 9500-9504, 9508), other specific malignant neoplasms, unspecific malignant neoplasms (8000-8005). Gliomas were also classified as astrocytic tumours (9384, 9400-9421, 9424, 9440-9442), oligodendroglial tumours and mixed gliomas (9382, 9450-9451), ependymal tumours (9383, 9391-9394) and other gliomas (9380-9381, 9423, 9430, 9444, 9460).
Due to the geographical differences observed for this cancer in Navarre, the area was also considered as an explanatory variable of the study. Navarre is a small region (644,477 inhabitants is 2011) and a third part of the population is concentrated in Pamplona (capital city) and hence most number of cases belong to the health areas of this city. Then, the observed cases were divided in two main areas: Pamplona, an urban area with more than 190,000 inhabitants (in the year 2012) and non-urban areas that correspond to the rest of Navarre.
Using the registered incident cases and resident populations, crude and age-standardized incidence annual rates of brain and CNS cancer per 100,000 person-years were calculated by the direct method separately by gender, urban and non-urban areas, year of diagnosis, and the following age-groups; 0-14, 15-44, 45-54, 55-64, 65-74 and, 75+. The world standard population was used as the reference population for age standardization. Assuming that age-standardized incidence annual rates are independent, averages of annual percentages of change (AAPC) were also computed between 1973 and 2008 for each category (gender, age-group and area). Age-standardized rate trends for morphological groups are also provided by quinquennia.
A temporal P-spline model was used to identify the age-standardized incidence rate temporal trend along the period 1973-2008 and the same model was used to forecast brain cancer incidence figures up to 2014. More precisely, predictions of incidence rates and counts by gender and age-groups were obtained. Based on this model incidence rates and new cases were obtained up to 2014, where counts were computed multiplying the forecast rates by projections of population data [21]. Let us defined the studied period as t= 1973…., 2008 the age-standardized rates (ASR) in each gender i and time t were modelled using a gender-specific model defined by
ASRit=fi(t)
while the following model was used to model the age-specific rate trends (AgSRat)
AgSRat = f(t) + fa(t)
In this expression f represents a common temporal trend for all age-groups and fi and fa are smooth functions to capture time trends in each gender and age-group respectively. These functions are estimated using the reformulation as linear mixed model of the P-splines. All the analyses were carried out using R 3.0.0 software [22].
Results
A total of 1755 incident cases of brain and other CNS cancer were identified among the 19,059,262 person-years covered by the registry from 1973 to 2008, which 996 occurred in men and 759 in women. In Table 1, the number of cases, person-years, age-standardized rates (ASR) and rates ratios are provided splitted by period (1973-1990 and 1991-2008), gender, area (urban and non-urban), and age-group. Annual percentage of change of rates and the corresponding CI-95% are also provided for the entire period. Overall, ASR increased from 6.461 to 7.033 cases per 100,000 person-years between 1973-1990 and 1991-2008. By gender, ASRs changed from 8.281 to 8.156 in male while in female rate increased from 4.790 to 5.923 between the periods mentioned before. By area, higher rates were observed in urban than non-urban areas during the entire period corresponding to an ASR ratio between urban and non-urban areas of 1.236 (CI95% 1.236-1.237) in 1973-1990 and, 1.126 (CI95% 1.125-1.126) in 1991-2008.
Brain cancer incidence rates and rate ration for the periods 1973-1990 and 1991-2008
| Period 1973-1990 | |||||||||
| Cases | Population | Rate (CI 95%) | Rate ratio (CI 95%) | ||||||
| Total | 715 | 9087581 | 6.461 | 6.460 | 6.463 | ||||
| Gender | Women | 272 | 4568870 | 4.790 | 4.788 | 4.792 | 1 | - | - |
| Men | 443 | 4518711 | 8.281 | 8.278 | 8.283 | 1.729 | 1.728 | 1.730 | |
| Area | Non-urban | 444 | 5960719 | 5.994 | 5.992 | 5.996 | 1 | - | - |
| Pamplona | 271 | 3126862 | 7.411 | 7.409 | 7.414 | 1.236 | 1.236 | 1.237 | |
| Age-group | 0-14 | 41 | 1068338 | 3.813 | 3.809 | 3.817 | 1.170 | 1,168 | 1,171 |
| Men | 15-44 | 66 | 1989544 | 3.259 | 3.256 | 3.261 | 1.00 | - | - |
| 45-54 | 74 | 533197 | 13.523 | 13.513 | 13.533 | 4.149 | 4,145 | 4,153 | |
| 55-64 | 130 | 448394 | 29.145 | 29.129 | 29.160 | 8.942 | 8,933 | 8,950 | |
| 65-74 | 83 | 310884 | 26.670 | 26.652 | 26.689 | 8.183 | 8,174 | 8,191 | |
| 75+ | 49 | 168354 | 27.202 | 27.178 | 27.227 | 8.346 | 8,336 | 8,356 | |
| Age-group | 0-14 | 24 | 1011666 | 2.279 | 2.276 | 2.282 | 0.887 | 0.886 | 0.889 |
| Women | 15-44 | 50 | 1899752 | 2.567 | 2.564 | 2.569 | 1.00 | - | - |
| 45-54 | 48 | 522153 | 8.829 | 8.821 | 8.837 | 3.439 | 3.435 | 3.443 | |
| 55-64 | 63 | 483605 | 13.039 | 13.029 | 13.049 | 5.079 | 5.073 | 5.085 | |
| 65-74 | 57 | 384512 | 14.771 | 14.759 | 14.783 | 5.754 | 5.747 | 5.761 | |
| 75+ | 30 | 267182 | 11.334 | 11.321 | 11.347 | 4.415 | 4.408 | 4.421 | |
| Period 1991-2008 | |||||||||
| Cases | Population | Rate (CI 95%) | Rate ratio (CI 95%) | ||||||
| Total | 1040 | 9971681 | 7.033 | 7.032 | 7.035 | ||||
| Gender | Women | 487 | 5010416 | 5.923 | 5.921 | 5.925 | 1 | - | - |
| Men | 553 | 4961265 | 8.154 | 8.151 | 8.156 | 1.377 | 1.376 | 1.377 | |
| Area | Non-urban | 639 | 6571484 | 6.735 | 6.733 | 6.737 | 1 | - | - |
| Pamplona | 401 | 3400197 | 7.582 | 7.579 | 7.585 | 1.126 | 1.125 | 1.126 | |
| Age-group | 0-14 | 33 | 752050 | 4.515 | 4.510 | 4.520 | 1.388 | 1.387 | 1.390 |
| Men | 15-44 | 80 | 2311684 | 3.251 | 3.248 | 3.253 | 1 | - | - |
| 45-54 | 84 | 642077 | 12.998 | 12.990 | 13.007 | 3.998 | 3.994 | 4.002 | |
| 55-64 | 100 | 523748 | 19.178 | 19.167 | 19.191 | 5.898 | 5.893 | 5.904 | |
| 65-74 | 147 | 428278 | 33.799 | 33.782 | 33.816 | 10.395 | 10.386 | 10.405 | |
| 75+ | 109 | 303428 | 35.091 | 35.070 | 35.112 | 10.793 | 10.783 | 10.803 | |
| Age-group | 0-14 | 16 | 704775 | 2.339 | 2.336 | 2.343 | 1.005 | 1.003 | 1.007 |
| Women | 15-44 | 55 | 2170401 | 2.327 | 2.324 | 2.328 | 1 | - | - |
| 45-54 | 49 | 618078 | 7.858 | 7.851 | 7.865 | 3.377 | 3.373 | 3.381 | |
| 55-64 | 94 | 527424 | 17.911 | 17.900 | 17.932 | 7.697 | 7.689 | 7.705 | |
| 65-74 | 128 | 488776 | 26.258 | 26.243 | 26.273 | 11.284 | 11.272 | 11.295 | |
| 75+ | 145 | 500962 | 29.310 | 29.294 | 29.325 | 12.595 | 12.583 | 12.608 | |
Regarding age-groups, differences were observed between the two periods and gender. In 1973-1990, males showed higher rates than women across the age-groups. Among men, the highest rates were observed for those aged between 55-64, 7.106 cases per 100,000 inhabitants, followed by 65-74 and 75+ age-groups. Among women, 65-74 age-group showed the highest rates, 5.754 cases per 100,000 inhabitants, followed by 55-64 and 75+ age-groups. In the period 1991-2008, women exhibited lower rates than men in all the age-groups, being the women older than 75 who showed the highest rate 12.595 cases per 100,000 inhabitants.
Table 2 shows the average annual percentage of change of overall brain cancer incidence rates. These results indicate a slightly increase of rates during 1973 to 2008 by an AAPC of 0.5% (CI95% 0.048%-1.005%). By gender, a significant increase of rates was also observed for women by an AAPC of 1.199% (CI95% 0.187%-2.220%). The AAPC was not significant for male. The increase was also significant among 65-74 and 75+ age-groups, for which the highest AAPC were observed, 2.605% (CI95% 1.016%-4.218%) and 5.885% (CI95% 3.215%-8.625%) respectively.
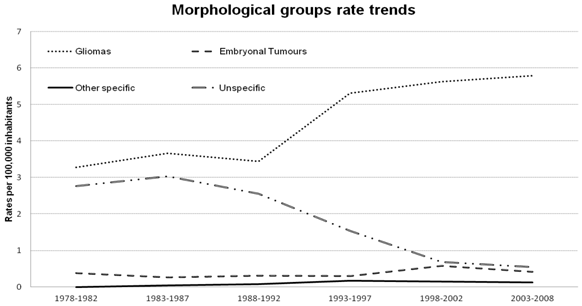
Figure 1 shows the brain and CNS cancer incidence rate trends by morphological groups between 1978 and 2008. A total of 1565 out of 1755 cases (89.17%) were classified according to their histology. In this figure a clear decrease of unspecific malignant neoplasms incidence rate is observed during the period, indicating an improvement in the histological classification of the cases. Gliomas were the most frequent neoplasm. In 2003-2008 the following rates per 100,000 inhabitants were observed for each morphological group: gliomas 5.795, unspecific malignant neoplasms 0.546, embryonal tumours 0.412 and other specific 0.120. In this last period 315 gliomas were identified from which 69.8% were astrocytic tumours, 7.9% were oligodendroglial tumours and mixed gliomas, 2.8% ependymal tumours and 19.7% were other gliomas.
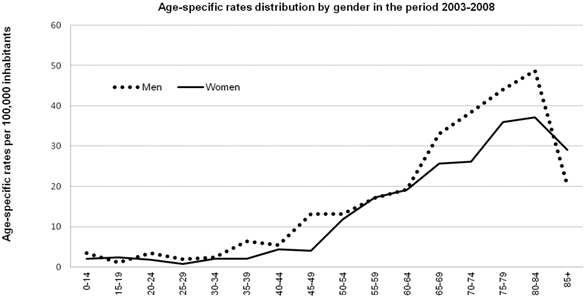
Figure 2 shows the age-specific incidence rates for the most recent 6-year period available (2003 through 2008) by gender. Children (0-14 years old) and adolescents (15-19 years old) showed the lowest rates in both genders with less than four cases per 100,000 inhabitants. Incidence rates increased slowly with age from young adults (35-39years old). After age 45 up to 84 years, rates increased sharply in both sexes, observing a decline for the oldest age group.
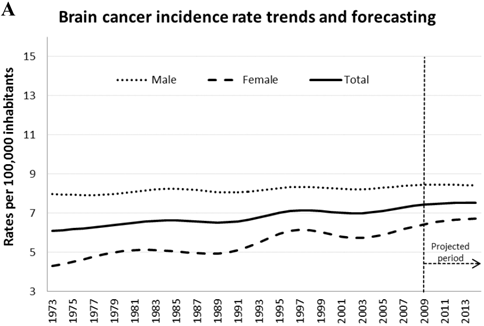
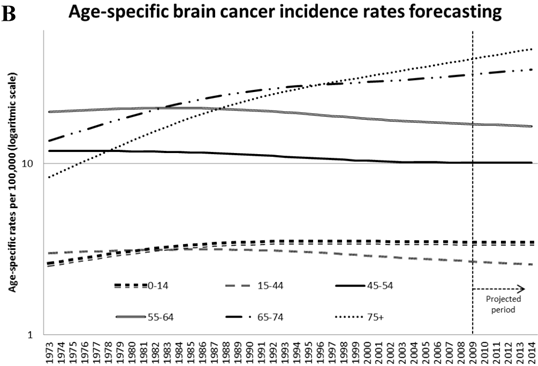
Figure 3 illustrates trends in age-standardized cancer incidence rates from 1973 to 2008 and the predicted rates for 2014 in men and women (Figure 3A). An increasing trend was observed for both sexes, more pronounced in female than in male. Figure 3B shows the age-specific rate trends along the studied period and forecasts for 2014. For those under 64 years old slightly reduction of age-specific rates are observed for the last years of the studied and forecast periods, while for the oldest age-groups (65+) a sharp increase in rate is shown. For 2014, 78 incident cases of brain cancer are predicted.
Average annual percent change (AAPC) in brain cancer incidence rates/100,000 person-years by gender, area and age-group between 1973 and 2008.
| Annual Percentage of change (CI 95%) between 1973-2008 | ||||
|---|---|---|---|---|
| AAPC | 95% Confidence Interval | |||
| Total | 0.525% | 0.048% | 1.005% | |
| Gender | Male | 0.140% | -0.491% | 0.776% |
| Female | 1.199% | 0.187% | 2.220% | |
| Area | Urban | 0.452% | -0.369% | 1.280% |
| Non-urban | 0.606% | 0.054% | 1.161% | |
| Age-group | 0-14 | 0.671% | -2.136% | 3.559% |
| 15-44 | -0.833% | -2.480% | 0.841% | |
| 45-54 | -0.493% | -1.433% | 0.456% | |
| 55-64 | -0.533% | -1.401% | 0.342% | |
| 65-74 | 2.605% | 1.016% | 4.218% | |
| 75+ | 5.885% | 3.215% | 8.625% | |
Trend of brain cancer and central nervous system incidence rates by morphological groups between 1973 and 2008.
Age-specific brain cancer incidence rates in the period 2003-2008.
A. Brain cancer incidence trend estimation and projections by gender. B. Brain cancer incidence trend estimation and projections by age-group.
Discussion
A total of 1755 incident cases of brain cancer were identified among 19,059,262 person-years covered by the cancer registry from 1973 to 2008 which involves one of the largest collections in time of brain cancer data in Spain. Age-specific rate analysis in the last six years pointed out that children and young adults had the lowest rates of brain cancer. The results also indicated that rates increase with age reaching the highest rate for 80-84 age-group, showing a slight decline for the oldest age-group (85+ years).
Incidence rates showed an increase trend along the studied period in which men showed higher incidence than women, although differences become smaller with time. This is consistent with results of other authors [4]. The projections indicate a slight increase in rates for 2014 in both sexed. Different hypothesis have been raised in the literature to explain gender differences. Some studies indicated that female sex hormones have a protective effect against brain cancer [23]. Others suggested innate differences in the susceptibility of X and Y chromosomes to tumourigenic stimuli [24,23], while others pointed out that these differences in gender could be explained by biological, social or lifestyle factors[25]. Our findings also showed a higher brain cancer incidence rates in urban areas (city of Pamplona) comparing with rural areas. Although many agricultural chemicals and pesticides used in rural areas are believed to be brain cancer risk factors, we could say that their effects in our region are small since the rates in rural areas are lower than in urban ones. Mobility of the population, mainly elderly people to urban areas, may be a reason for these differences between urban and rural incidence rates. Our incidence data only provides the residence of the patients at the time of diagnosis. We do not consider information about previous residences. Other studies have considered the air quality, air pollution or level of industrial development as factors that could explain differences between urban and rural areas [23,26], but in our study we do not have data to assess these risk factors. Incidence rate trends by histological type of brain and CNS cancer indicated an increase of gliomas and a clear decrease of unspecific malignant neoplasms in the last years. These results are consistent with the finding of other [23].
The improvement on diagnostic techniques allows a more specific diagnosis of this tumour, which could have a double effect on the trends. On the one hand, improvement of diagnostic rate could lead a better morphological classification of these cancers reducing the number of unspecific malignant neoplasms. On the other hand, these techniques have contributed to a better coding of possible brain metastases that formerly could be classified as brain tumours. This could affect the trend in the opposite direction.
Some studies suggested that an exposure to electromagnetic fields or the use of mobile phones could be in association with brain cancer development. But most of the studies conclude that the association is small or non-significant. It has been also indicated that hereditary syndromes, diet and vitamins play an important role in adult brain cancers [27]. Neither diet, tobacco smoking or alcohol consumption has been found strongly associated with increased risk or protective effects for brain cancer in adults [28]. The brain cancer incidence rate has increased in recent years in the industrialized countries and survival is generally poor compared to many other cancers [29].
The population-based Navarre Cancer Registry was one of the pioneers in Spain starting into operation in 1970 [18] and it has an important role in cancer control, teaching, research and publishing regional cancer figures providing useful and reliable incidence information of different cancer types. This registry contributes to the Cancer Incidence in Five Continents (CI5) series edited by the International Agency for Research on Cancer (IARC). It means that this cancer registry fulfills all quality-criteria and quality-control procedures to produce reliable and unbiased data. One of the limitations of population-based cancer statistics is that data on cancer incidence is available to the general public after approximately three or four years due to administrative and procedural delays. This means that 2014 cancer data will be available in 2018, and then, there is a gap between the present time and the data available. In that context, four-year predictions on brain cancer incidence are provided based on temporal P-spline models. Accurate forecast figures allow public health workers to prioritize prevention activities, to allocate health services, and to evaluate the impact of certain interventions up to date. Different methods have been used in the literature in order to forecast cancer incidence mortality figures. For example, logarithmic Poisson count data joinpoint models, simple log-linear trends, age-period-cohort models or autoregressive time series among others. The P-spline model is appropriate to capture smooth temporal trends and to predict cancer incidence figures in different groups or areas. A spatio-temporal version of the P-spline model has been already used in the literature to smoothing and forecasting prostate cancer mortality risks in all the Spanish provinces within the oncoming years [30].
To summarize, age-adjusted incidence rates for brain cancer showed an increase over the study and forecast period in both sexes. This increase is mainly a reflection of the increase of rates in the oldest age groups since the rates for younger age groups remained stable or decreased over time. Few causal factors are established as a brain cancer risk factor and many others have been hypothesized. In this context it is necessary to continue promoting healthful lifestyles for primary prevention among all the population of Navarre.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No.11; Lyon, France: International Agency for Research on Cancer; 2013. http://globocan.iarc.fr
2. Ardanaz E, Azagra MJ, San Román E, Burgui R, Barricarte A. Cancer Incidence in Navarre (2003-2007). In: Forman D, Bray F, Brewster DH, Gombe Mbalawa C, Kohler B, Piñeros M, Steliarova-Foucher E, Swaminathan R and Ferlay J. Cancer Incidence in Five Continents, Vol X (electronic version) Lyon, IARC. http://ci5.iarc.fr
3. López-Abente G, Ramis R, Pollán M, Aragonés N, Pérez-Gómez B, Gómez-Barroso D. et al. Atlas municipal de mortalidad por cáncer en España, 1989-1998. Madrid, Spain: Instituto de Salud Carlos III. 2006
4. Ruiz-Tovar M, López-Abente G, Pollán M, Aragonés N, Ardanaz E, Moreo P, Moreno C, Vergara A. Brain cancer incidence in the provinces of Zaragoza and Navarre (Spain): effect of age, period and birth cohort. J Neurol Sci. 1999;164(1):93-99
5. López-Abente G, Pollán M, Ardanaz E, Errezola M. Geographical pattern of brain cancer incidence in the Navarre and Basque Country regions of Spain. Occup Environ Med. 2003;60:504-508
6. Preston MS. Epidemiology of primary CNS neoplasms. Neurol Clin. 1996;14:273-90
7. Fang Z, Kulldorff M, Gregorio D. Brain cancer mortality in the United States, 1986 to 1995: A geographic analysis. Neuro Oncol. 2004;6(3):179-187
8. Bondy M, Wiencke J, Wrensch M, Kyritsis AP. Genetics of primary brain tumors: A review. J Neurooncol. 1994;18:69-81
9. Thomas TL, Inskip PD. Brain and other nervous system. Cancer Rates and Risks, 4th Ed. Bethesda, MD: National Institutes of Health, National Cancer Institute. 1996:114-119
10. Preston-Martin S, Lewis S, Winkelmann R, Borman B, Auld J, Pearce N. Descriptive epidemiology of primary cancer of the brain, cranial nerves, and cranial meninges in New Zealand, 1948-88. Cancer Causes Control. 1993;4(6):529-38
11. Demers PA, Vaughan TL, Schommer RR. Occupation, socioeconomic status, and brain tumor mortality: a death certificate-based case-control study. J Occup Med. 1991;33(9):1001-1006
12. Orfeuvre H, Lutz JM, Menegoz F, Exbrayat C, Colonna M, Schaerer R. Incidents of brain tumors observed in the Grenoble area (canton of Meylan) 1979-1990. Rev Neurol Paris. 1993;149(5):340-344
13. Eaton N, Shaddick G, Elliott P. Small-area study of the incidence of neoplasms of the brain and central nervous system among adults in the West Midlands Region, 1974-86. Br J Cancer. 1997;75(7):1080-1083
14. El País. Anuario 1996. País, Madrid: Ediciones El. 1996
15. de Crédito BE. Anuario del Mercado Español 1991. Madrid: Banco Español de Crédito. 1991
16. Frei P, Poulsen AH, Johansen C, Olsen JH, Steding-Jessen M, Schüz J. Use of mobile phones and risk of brain tumours: update of Danish cohort study. BMJ. 2011;343:d6387 doi: 10.1136/bmj.d6387
17. González J, Gorgojo L, Martín J, Villar F. Cáncer en España. Ministerio de Sanidad y Consumo, Madrid. 1993
18. Navarro C, Martos C, Ardanaz E, Galceran J, Izarzugaza I, Peris-Bonet R, Martínez C, the Spanish Cancer Registries Working Group. Population-based cancer registries in Spain and their role in cancer control. Ann Oncol. 2010;21(3):iii3-iii13
19. WHO. Classifications. International Classification of Diseases (ICD). http://apps.who.int/classifications/icd10/browse/2010/en
20. Statistical Institute of Navarra. http://www.navarra.es/AppsExt/GN.InstitutoEstadistica.Web/InformacionEstadistica.aspx?R=1E=1
21. Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Boyle P. Cancer Incidence in Five Continents, Vol IX. Lyon, IARC: IARC Scientific Publications No 160. 2007
22. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org
23. Deorah S, Lynch CF, Sibenaller ZA, Ryken TC. Trends in brain cancer incidence and survival in the United States: Surveillance, Epidemiology, and End Results Program, 1973 to 2001. Neurosurg Focus. 2006;20(4):15
24. Johnson DR, Leeper HE, Uhm JH. Glioblastoma survival in the United States improved after Food and Drug Administration approval of bevacizumab: A population-based analysis. Cancer. 2013;119(19):3489-3495
25. Blowers L, Mack W, Preston-Martin S. Dietary and other lifestyle factors of women with brain gliomas in Los Angeles County (California, USA). Cancer Causes & Control. 1997;8:5-12
26. Gomes J, Zayady A. Occupational and Environmental Risk Factors of Adult Primary Brain Cancers. A systematic Review. Int J Occup Environ Med. 2011;2(2):82-111
27. Wrensch M, Minn Y, Chew T, Bondy M, Berger MS. Epidemiology of primary brain tumors: Current concepts and review of the literature. Neuro Oncol. 2002;4(4):278-299
28. Inskip PD, Linet MS, Heineman EF. Etiology of brain tumors in adults. Epidemiol Rev. 1995;17:382-414
29. De Angelis R, Sant M, Coleman MP. et al. Cancer survival in Europe 1999-2007 by country and age: results of EUROCARE-5-a population-based study. Lancet Oncology. 2014;15:23-34
30. Ugarte MD, Goicoa T, Etxeberria J, Militino AF. Projections of cancer mortality risks using spatio-temporal P-spline models. Stat Methods Med Res. 2012;21(5):545-560
Author contact
![]() Corresponding author: Eva Ardanaz, Navarre Cancer Registry, Epidemiology Unit, Navarre Public Health Institute, Calle Leyre 15, 31006 Pamplona, Spain. E-mail: me.ardanaz.aicuaes
Corresponding author: Eva Ardanaz, Navarre Cancer Registry, Epidemiology Unit, Navarre Public Health Institute, Calle Leyre 15, 31006 Pamplona, Spain. E-mail: me.ardanaz.aicuaes

 Global reach, higher impact
Global reach, higher impact