3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(15):2889-2894. doi:10.7150/jca.86582 This issue Cite
Research Paper
Clinical Significance of Preoperative Assessment of Intravesical Prostatic Protrusion in Radical Prostatectomy
1. Department of Anesthesiology, Zhongshan Hospital, Fudan University, Shanghai 200032, China.
2. Department of Urology, Zhongshan Hospital, Fudan University, Shanghai 200032, China.
3. Department of Urology, Zhongshan Hospital Wusong Branch, Fudan University, Shanghai 200940, China.
Jie Tang, Wei Xi, and Yanjun Zhu contributed equally to the work.
Abstract
Background: Intravesical prostatic protrusion (IPP) is common in prostate-related diseases, whose clinical significance in radical prostatectomy was unknown.
Methods: 791 patients underwent robot-assisted or open radical prostatectomy at our institution were enrolled. The transabdominal ultrasound examination of prostate and IPP was carried out preoperatively, by which IPP was classified as no (0-0.5cm, grade 0), slight (0.6-1.0cm, grade 1) and noticeable (>1.0cm, grade 2).
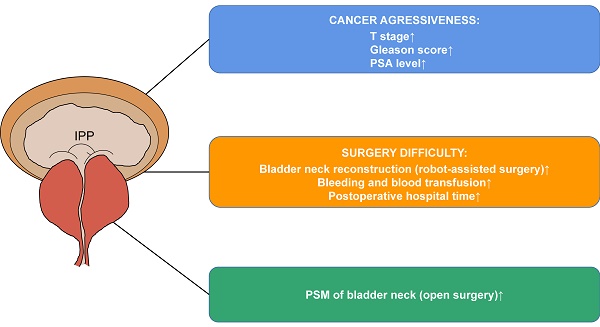
Results: 185 (23.4%), 170 (21.5%) and 436 (55.1%) patients had no, slight and noticeable IPP, respectively. Generally, prostate specific antigen (PSA), Gleason score and pT stage increased with IPP grade. In particular, cases with grade 0 IPP had a decreased proportion of seminal vesicles' involvement than those with grade 1 and grade 2 IPP (p=0.035). Reconstruction of the bladder neck (in robot-assisted group), increased surgical bleeding (>200ml), and prolonged postoperative hospital stays (>14 days) happened more in patients with grade 2 IPP. Blood transfusion only happened in patients with noticeable IPP. PSM of bladder neck was only associated with higher IPP grade in open surgery group (p=0.032), not in robot-assisted surgery group.
Conclusion: IPP is associated with cancer aggressiveness, surgery difficulty and PSM of bladder neck in prostate cancer. Assessment of it provides more information for operations.
Keywords: prostate cancer, intravesical prostatic protrusion, prostate-bladder junction, clinical significance, surgical margin of bladder neck.

 Global reach, higher impact
Global reach, higher impact