3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(4):908-915. doi:10.7150/jca.91169 This issue Cite
Research Paper
EBUS-TBLC increase the diagnosis rate in different type of peripheral pulmonary lesions
1. Department of Respiratory and Critical Care Medicine, The Huaian Clinical College of Xuzhou Medical University, Huai'an 223300, China.
2. Research Center for the prevention and treatment of drug resistant microbial infecting, Youjiang Medical University for Nationalities, Baise 533000, China.
3. Department of Pathology, the Affiliated Nanjing Hospital of Nanjing Medical University, Nanjing 210006, China.
4. Department of Respiratory and Critical Care Medicine, The Affiliated Huaian No.1 People's Hospital of Nanjing Medical University, Huai'an 223300, China.
5. Department of Pathology, The Affiliated Huaian No.1 People's Hospital of Nanjing Medical University, Huai'an 223300, China.
6. Department of Respiratory and Critical Care Medicine, The First Affiliated Hospital of Naval Medical University, Shanghai, China.
7. Pulmonary Department, Bioclinic Private Clinic, Aristotle University of Thessaloniki, Thessaloniki, Greece.
8. 2 ND Surgery Department, University General Hospital of Alexandroupolis, Democritus University of Thrace, Alexandroupolis, Greece.
9. Pathology Department, University of Cyprus, Cyprus.
Abstract
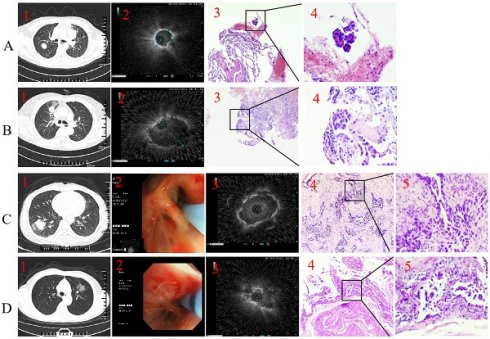
Background and objective: Recently, endobronchial ultrasonography with guide sheath-guided (EBUS-GS) has been increasingly used in the diagnosis of peripheral pulmonary lesions (PPLs) from human natural orifice. However, the diagnostic rate is still largely dependent on the location of the lesion and the probe. Here, we reported a new procedure to improve the diagnostic rate of EBUS-transbronchial lung cryobiopsy (EBUS-TBLC), which performed under general anesthesia with laryngeal mask airway (LMA) in all of the patients. This study retrospectively evaluated the diagnosis of PPLs with 'blind-ending' type (Type I) and 'pass-through' type procedures (Type II) of EBUS-GS-TBLB or EBUS-TBLC respectively.
Methods: Retrospective review of 136 cases performed by EBUS-GS-TBLB or EBUS-TBLC for PPLs over 2 years.
Results: A total of 126 cases EBUS-GS-TBLB or EBUS-TBLC were performed during the study period. Among them, 66 (52.4%) were performed Type I and 60 (47.6%) were performed Type II. Clinical baseline characteristics did not differ between two groups. The overall diagnosis rate of 126 patients with EBUS-GS-TBLB or EBUS-TBLC was 73% (92/126), and different method type have significant influence on the diagnostic yield (P = 0.012, x2 = 4.699). Among them, diagnostic yields for Type I with forceps biopsy (n=34), Type I with cryobiopsy (n=32), Type II with forceps biopsy (n=30), and Type II with cryobiopsy (n=30) were 72.5%, 64.5%, 70.4% and 74.2% respectively (Figure 2A). The study further compared the outcomes of different procedures in concentric and eccentric lesion. Diagnostic yields for Type I with eccentric (n=30), Type I with concentric (n=36), Type II with eccentric (n=34), and Type II with concentric (n=26) were 58.2%, 76.9%, 60.2% and 74.8%, respectively (P < 0.05). The incidence of complications in 126 patients was 2.6%.
Conclusion: EBUS-GS-TBLB and EBUS-TBLC both are very safe and highly diagnostic technique; different method types have significant influence on the diagnostic yield. Moreover, Type II procedure has higher diagnostic yield. In addition, Type I with eccentric had the lowest diagnosis yield.
Keywords: EBUS, PPLs, type, eccentric, concentric.

 Global reach, higher impact
Global reach, higher impact