3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(6):1668-1674. doi:10.7150/jca.92689 This issue Cite
Research Paper
The efficacy of cetuximab plus PD-1 inhibitors as salvage therapy in PD-1 refractory patients with recurrent or metastatic head and neck squamous cell carcinoma
1. School of Stomatology, Weifang Medical University, Weifang, China.
2. Department of Oral Maxillofacial-Head and Neck Oncology, Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China.
3. Shanghai Key Laboratory of Stomatology & Shanghai Research Institute of Stomatology; National Clinical Research Center of Stomatology, Shanghai, China.
4. National Clinical Research Center of Stomatology, Shanghai, China.
# These authors contributed equally to this work and should be considered co-first authors.
Abstract
Purpose: The prognosis of patients with recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC) that are refractory to programmed cell death protein 1 (PD-1) immunotherapy is relatively poor. The salvage therapy was rarely investigated and urgently needed.
Methods: We conducted a single center retrospective real-world study to explore the efficacy of cetuximab plus PD-1 inhibitors as salvage therapy in patients progressed from first-line immunotherapy.
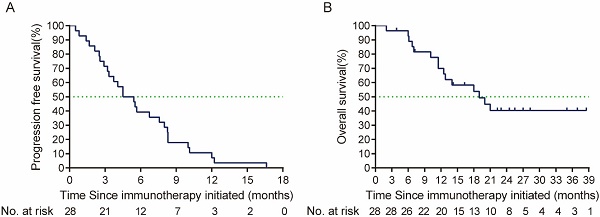
Results: In the present study, 28 eligible patients were included between October 2020 and May 2023. By the cut-off date (Sep 24th, 2023), the objective response rate (ORR) was 46.4% (95% CI, 29.5%-64.2%). Kaplan-Meier survival analysis revealed the median progression free survival (mPFS) in the study was 6.87 months (95% CI, 4.77-8.97 months), and median overall survival (mOS) was 9.67 months (95% CI, 4.79-14.55 months). Multivariate Cox regression analysis indicated that ECOG performance status and best response to salvage therapy was found to be the prognosis factor of salvage therapy. For the safety, the most common treatment related adverse events (TRAEs) were rash (72.1%), anemia (64.3%) and fatigue (46.5%) during the salvage therapy. The most common potential irAEs were hypothyroidism (25%), and pneumonitis (14.3%). Only 3 patients (10.7%) experienced grade 3 TRAEs, and no treatment-related deaths occurred.
Conclusions: Our study showed the combination of cetuximab with PD-1 inhibitors might be a potential efficacy and safety choice in PD-1 refractory patients with R/M HNSCC which need further investigation.
Keywords: programmed cell death protein 1 (PD-1) immunotherapy, cetuximab, salvage therapy, recurrent or metastatic head and neck squamous cell carcinoma (R/M HNSCC)

 Global reach, higher impact
Global reach, higher impact