Impact Factor
ISSN: 1837-9664
J Cancer 2010; 1:112-119. doi:10.7150/jca.1.112 This volume Cite
Short Research Communication
Practice and Effectiveness of Outpatient Psycho-Oncological Counseling for Cancer Patients
1. Charité Comprehensive Cancer Center, Berlin, Germany
2. Berliner Krebsgesellschaft e.V., Berlin, Germany
3. SOSTANA, Berlin, Germany
Received 2010-7-13; Accepted 2010-8-23; Published 2010-8-23
Abstract
Objective: Because of various types of psychological distress, cancer patients are encouraged to attend outpatient psycho-oncological and psychosocial counseling. The aim of this prospective study was an analysis of the impact and success of existing counseling resources.
Methods: All cancer patients who had applied at a central counseling center were given a standardized questionnaire (FBK-R23), designed to assess the type and degree of cancer patients' difficulties prior to their first counseling session. Additionally, the psychological condition of the patients was assessed psycho-oncologically by a third party (PO-Bado). After at least 2 and no more than 5 sessions, patients underwent both self-evaluation and third-party assessment, using the same instruments.
Results: During the period from September 2008 and August 2009, we looked at a total of 447 people seeking counseling, including 186 family members (42%), 33 professional caregivers (7%), and 228 patients (51%). Out of the 228 patients, 48 attended our counseling sessions personally and 20 of these additionally completed the second questionnaire. Counseling led to only a tendency toward improvement, on average, of total psychological distress (p=0.08). In individual areas - for example, “Social Distress” and “Everyday Limitations”- no change could be measured. Only the problem area identified as “Information Deficit” was improved, on average, after 3 counseling sessions (p=0.008).
Conclusion: Our results indicate that while short-term counseling has no concrete effect on the improvement of a patient's psychological well-being, these support sessions do serve to decrease the patient's so-called “Information Deficit”, thereby bringing about an indirect improvement in the sufferer's psychological state. The course of treatment offered should be determined according to the patient's needs. In order to ensure that even the very sickest of the tumor patient group seek outreach groups, we must target this particular group with additional evaluative questions. Further studies must determine whether short-term counseling or other counseling strategies are most effective.
Keywords: cancer, oncology, psycho-oncological counseling, distress, support
Introduction
According to figures from the World Health Organization (WHO), each year more than 11 million people fall ill with cancer, and 7.9 million die from the disease. Cancer, therefore, is the world's second-most frequent cause of death. The diagnosis alone of a malignant cancer can cause an existential crisis for the patient [1]. The most significant physical, psychological, and social distress that accompany an oncological illness are the patient's loss of a sense of physical inviolability, the menace of death, loss of autonomy, and social isolation [2]. The degree to which psychological co-morbidities impact patient health has been shown to have extensive variability in data from the relevant literature. Depending on treatment phase, these numbers lie between 29% and 77% [3]. Psychological distress can appear at any point in the course of the illness. On the one hand, it is a reaction to the oncological illness itself. On the other hand, it can also come about as a result of treatments, which are also difficult. Not least, familial and professional distress can result as well. But damage attributable to the medical care system itself also has an impact on cancer patients [4]. Consequent needs for information about the illness and treatment options arise, as does the desire for a participatory decision-making process [5]. Psycho-oncology as an integral part of oncology is an idea that has become internationally recognized, though it has only been implemented as a standard part of the medical care routine in some countries [6]. Psycho-oncological treatments are offered in varying situations. Support could be important in acute treatment phases, rehabilitation, and follow-up care. In some cases, screening is recommended as soon as a diagnosis is delivered [7]. According to data from the Comprehensive Cancer Network, only some 5% of severely affected patients in the USA receive psycho-oncological help [8]. The effects of psycho-oncological support have been demonstrated in various studies on cancer patients treated both in group and individual therapies [9]. The spectrum of such therapies ranges from psycho-educative measures to psychotherapeutic interventions [10]. Even short and limited measures can achieve an improvement of the patient's psychological wellbeing [11]. Ultimately, the quality of life of the patient can be positively influenced with the help of psycho-oncological interventions [9, 12-14]. Currently, it remains unclear whether the offer of outpatient psycho-oncological treatment has an influence on the psychological condition of the cancer patient. Which areas are most affected, and can changes in various areas be measured? If one assumes that highly-distressed self-actualizing patients will find their way to an ambulant psychological therapy resource on their own, then the question must be asked: how do the self- and third-party assessments of these patients' distress levels look before and after the therapy's end point?
Method
Study design
All advice-seekers who contacted the Berlin Cancer Society's psycho-oncological and psycho-social counseling center for an initial counseling session were included in a screening list. Only advice-seekers who were themselves sick with cancer were informed, orally and in writing, of the substance and aims of the examination. Study protocol, patient information and consent forms were approved by the Charité Hospital's Ethics Committee, under code EA3/003/08. The study is subject to the Helsinki Declaration as well as data privacy protection laws.
After the patients had consented in writing to participate, they were asked to fill out a standardized questionnaire (FBK-R23) that assesses a cancer patient's distress levels. Prior to the first counseling session, an assessment of the patient's subjective distress was conducted using psycho-oncological base-documentation (PO-Bado). This assessment was conducted without the counselor being given access to the patient's self-assessment materials. According to the needs of the patient, psycho-oncological and psycho-social counseling followed. One counseling session lasts about one hour. The time that elapses between sessions should not exceed 6 weeks. After at least 2 and not more than 5 sessions, the patients were again asked to self-assess their distress levels. The third party assessment of the subjectively experienced distress after the counseling period was conducted by an external psycho-oncologist to prevent this assessment from being influenced by the prior counseling sessions.
Participants
In the time period from September 2008 and August 2009, 447 first-time advice seekers consulted the counseling center. Among that group were 228 patients with an oncological illness (51%), 186 family members (42%), and 33 professional caregivers (7%). Of the 228 cancer patients, 105 (46%) came to the counseling center in person, and 123 patients (54%) contacted the center by telephone or in writing. 52 of the patients who came in person to the counseling center were not eligible for the study. Reasons for ineligibility included inadequate German language skills, the desire for a one-time consultation only, or cases of crisis intervention. 5 patients chose not to participate in the study. Consequently, 48 patients who fulfilled the study's criteria consented in writing to participate. The sample group was composed of 15 men (31%) and 33 women (69%). The average age was 51 years (SD=12). The patients ranged in age from 26 to 79 years. Women with breast cancer were most common (N=17; 35%). Second most common were men with urological tumors (N=7; 15%). The group as a whole included patients with solid tumors as well as blood cancers. After at least 2 and no more than 5 counseling sessions, patients were asked to fill out the FBK-R23 once again. This was followed by an assessment of the patient's condition, performed by an independent psycho-oncologist not employed by the counseling center. The time that elapsed between counseling sessions was not allowed to exceed 6 weeks. A total of 16 of the 48 patients broke off contact with the counseling center within the observation period.
The proscribed time period of 6 weeks was exceeded by 9 patients and 3 patients died. Consequently, 20 patients were able to participate in the study's final evaluation. This sample group consisted of 5 men (25%) and 15 women (75%). The average age was 52 years (SD=13). The youngest patient was 26 and the oldest 79. In this group, women with breast cancer were still the majority, making up 40% of the group (N=8). A description of the sample group can be found in Table 1.
Sociodemographic and medical characteristics of the study participants.
| n=20 | % | |
| Age | ||
| Arithmetic mean in years (range) (SD) | 51.85 (26-79) (SD=13.30) | |
| Sex | ||
| male | 5 | 25.0% |
| female | 15 | 75.0% |
| Partner | ||
| yes | 11 | 55.0% |
| no | 9 | 45.0% |
| Children | ||
| yes | 15 | 75.0% |
| no | 5 | 25.0% |
| unknown | 0 | 0.0% |
| Diagnosis | ||
| breast cancer | 8 | 40.0% |
| urological tumor | 4 | 20.0% |
| gynaecological tumor | 2 | 10.0% |
| skin tumor | 1 | 5.0% |
| gastric-, oesophageal-, pancreatic tumor | 1 | 5.0% |
| haematological malignancies | 2 | 10.0% |
| other | 2 | 10.0% |
| Disease status | ||
| primary tumor | 15 | 75.0% |
| follow up | 1 | 5.0% |
| relapse | 3 | 15.0% |
| second malignancy | 1 | 5.0% |
| not evaluable | 0 | 0.0% |
| Treatment in the last 2 months (More than one answer possible) | ||
| chemotherapy | 4 | 20.0% |
| none | 0 | 0.0% |
| hormonal therapy | 5 | 25.0% |
| radiation | 4 | 20.0% |
| surgical procedure | 3 | 15.0% |
| other | 6 | 30.0% |
Measures
Questionnaire regarding cancer patients' distress levels (FBK-R23)
The questionnaire regarding cancer patients' distress levels (FBK-R23) is a psychometrically proven test that serves to ascertain and quantify the psycho-social aspects of distress undergone by patients with cancer [15]. It covers all tumor diagnoses, stages, and treatments. The test can be used to screen psycho-oncological distress for the purposes of clinical monitoring and therapy evaluation. The questionnaire contains 23 statements that were compiled such that 5 distinct areas of psycho-oncological distress can be examined. These areas are organized into the following charts: “Psychosomatic Distress” (5 items), “Anxiety” (4 items), “Information Deficit” (4 items), “Restrictions on Daily Life” (5 items) and “Social Distress” (5 items). The patients are asked to decide whether certain situations apply to them or not. Should one or more distress situation apply, patients are then asked to determine the degree to which they are affected according to 5 categories, from “Applies and does not distress me much”(1) to “Applies and distresses me very intensely”(5). The time required for the patient to fill out the questionnaire is about 10 minutes. The analysis of the individual charts occurs through the formation of the mean. The patient's total distress level is calculated using the sum total of all the items. The objectives for implementation and scoring are given. The homogeneity of the charts lies between 0.65 and 0.80. The internal consistency of the entire questionnaire is rated "very good", with alpha= .89 [16].
Psycho-oncological Base Documentation (PO-Bado)
A questionnaire for third-party evaluation of the cancer patient's subjective condition has existed since 2004 as part of the psycho-oncological base documentation [17]. The patients' experience, in regard to “Somatic Distress” (4 items) and “Psychological Distress” (8 items), was obtained and compiled in the last 3 days of the study period. In this manner the subjective condition and not the intensity of the symptoms is ascertained. The evaluation, using a 5-tiered rating scale, follows. Potential additional distress factors are assessed with 3 items. Most important of these are social issues. In addition, it is assessed whether the patient's psychological condition is influenced by factors unrelated to the illness itself. These interviews last for 20 minutes.
Counseling topics
With the help of a standardized questionnaire developed in-house, we collected information regarding both the primary concerns of the patients as well as the substance of the counseling sessions. Primary concerns were: Information about psychotherapy or psycho-oncological counseling, supervision, support, coming to terms, death and dying, crisis situations, financial problems, information about social law issues, self-help, family and partner relations, medical questions, rehabilitation, and miscellaneous other issues. Counseling topics included: Information, crisis intervention, basic psychotherapeutic services, social issues, and miscellaneous other issues. In addition, the patient's further development is measured: Psychotherapy, self-help groups, medical advice, and miscellaneous other issues. The documentation was carried out by the counselor, and multiple answers were possible.
Statistical Analyses
Results were expressed as arithmetic mean with standard deviation (SD) and frequencies with percentage, respectively. After proof of the distributions for normality, differences between the regarded groups in terms of interesting clinical parameters were tested by using either the (paired) t-test or the (paired) non-parametric Wilcoxon-test. In that sense, a change in the patients' total distress level before and after the intervention (measured in terms of the patient's self analyses) and the effectiveness of counseling (in terms of the third-party assessment) were verified. Agreement was judged calculating Cohen's kappa (κ), tested for non-association (κ = 0) and interpreted by using the categories of Landis and Koch [18]. Furthermore, symmetry was tested by the pair-wise McNemar-test. In case of small samples, greater differences in sample sizes, large but unbalanced groups, data sets containing ties, or sparse data, tests were carried out in an exact version. A p-value < 0.05 was considered statistically significant. All statistical tests were conducted in the area of exploratory data analyses. Therefore, no adjustments for multiple testing have been made. Numerical calculations were performed with SPSS, Version 17, copyright SPSS, Inc., Chicago, Illinois 60606, USA.
Results
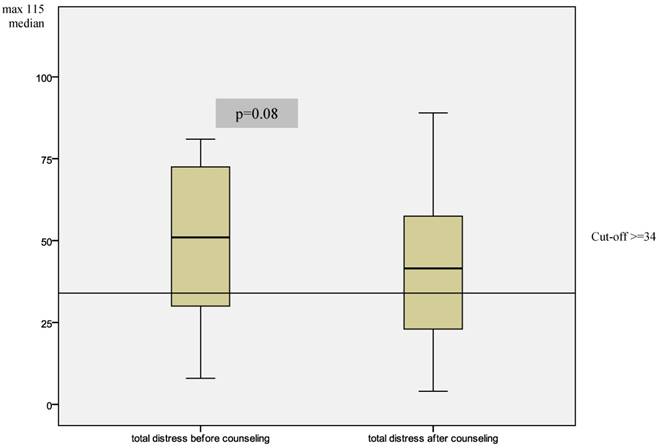
The substance of the counseling interview was documented and evaluated. In a single session, several thematic areas might be worked on with the counselor. Frequently discussed were questions concerning help with working through the illness (85%). Just as frequently discussed were concrete questions concerning working through the aftermath of illness and treatment (65%). Problems with family and partner relations were raised by 70% of patients, questions about rehabilitation measures by 50% of patients, and social law difficulties were an issue for 30% of patients. The average number of counseling sessions attended was 3 per patient. The minimum number of counseling sessions was 2, and 5 patients attended only 2 sessions, while 1 patient attended 5 sessions. From the standpoint of patients' self-assessments, the overall psychological distress they experienced was reduced on average from 49.3 to 42.75 (p=0.08). Differences are designated according to the individual sub-scale shown in figure 1. The problem areas “Daily Life Restrictions” and “Social Distress” changed only negligibly during the period during which patients underwent counseling sessions (figure 2).
Changes in patients' self-evaluated total distress levels before and after counseling.
Changes in single areas of distress from the viewpoint of the patients before and after counseling.
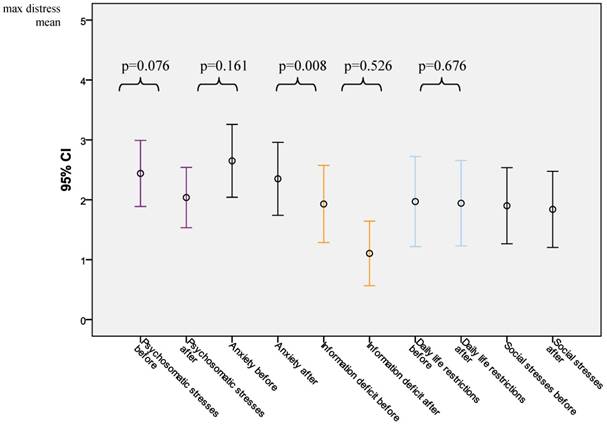
Before counseling, “Daily Life Restrictions” rated on average 1.97, and after counseling, 1.94 (p=0.526). Prior to counseling, “Social Distress” rated on average 1.90 and 1.84 afterwards (p=0.676). On the other hand, within the category “Psychosomatic Distress” a tendency towards improvement can be seen. The average valuation decreased from 2.44 to 2.04 (p=0.076). A similar decrease was observable in the category “Anxiety”. Here, the average value decreased from 2.65 before the counseling sessions to 2.35 after counseling (p=0.161). Most clear was the improvement in regards to “Information Deficit”. Before counseling, this category's values were 1.93, but these sunk to 1.10 (p=0.008). When comparing the pre-counseling self-assessments from patients who went on to have only one counseling session with pre-counseling self-assessments of patients who went on to have multiple sessions, no significant difference between the characterized distress could be found. Patients who had a single session tended to be less anxious (p=0.2) and also tended to have higher “Information Deficit” (p=0.2). The effects of counseling as measured by the third-party analysis on the degree of improvement in distress levels are shown in figure 3. The “Somatic Distress” decreased from 5.70 to 3.85 (p=0.154). In the analysis, “Psychological Distress” underwent a clear improvement. The average value sank from 17.15 to 10.45 (p=0.001). Comparisons were also made between the self-analyses and the third-party analyses of distress levels. 15 patients (75%) assessed their distress levels before counseling at higher than the cut-off valuations. The third-party evaluation rated by using cut-off scores all 20 patients (100%) as having high psycho-oncological distress. No statistics (neither kappa nor McNemar) were computed because variable “third-party” is a constant.
Changes in levels of distress before and after counselling as evaluated by the third party.
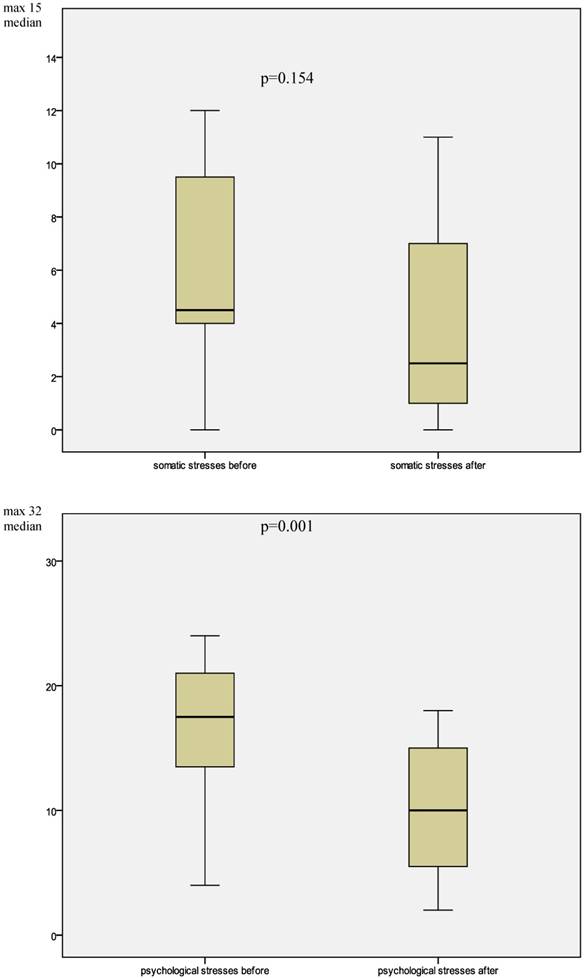
After the counseling period's end, in self-evaluation that number decreased to 12 patients (60%). Now 15 patients (75%) were still rated as highly distressed. There are a “good” overall agreement (kappa = 0.667), and symmetry in the judgments cannot be rejected (McNemar's p = 0.250).
Discussion
The main aim of the study was to clarify the question of whether or not measurable changes in individual areas of a patient's psychological condition take place after outpatient psycho-oncological and psycho-social counseling. Patients' self-assessed distress levels decreased only tendentially at the end of the counseling process. For this change to occur, 3 sessions were necessary, on average. Individual distress areas underwent neither improvement nor decline during the observation period. Only the area of “Information Deficit” underwent a significant improvement. According to the assessments of various occupational groups, patients lacked information. What emerged was a consensus that patients didn't feel they had received adequate education regarding their illness and treatment options. As a result, patients sought out different doctors and were potentially confronted with differing opinions. Furthermore, patients felt that they received inadequate information regarding possibilities for social and financial support. A further information deficit consisted of the feeling that inadequate information was relayed regarding the availability of profession counselors to discuss emotional problems stemming from the diagnosis.
Through counseling sessions, the number of distressed patients decreased, according to both the patients' self-assessments and third-party assessment. In self-assessments, the number of distressed patients sank from 15 to 12, and according to the third-party analyses, this number was reduced from 20 to 15. Differences regarding the measurement of psychological distress in oncological patients are established in the literature on the topic [19, 20].
Of particular note is the high number of family members who come to the counseling center. This underscores the assertion that the family of the cancer patient also experiences considerable detriment to its psychological health [21, 22]. Only about half of the advice-seekers are patients. For many of them, a single counseling session seemed to be adequate. Whether further counseling or psychotherapy was subsequently sought in another counseling center by this sub-group cannot be determined through our findings. Nor can we determine whether or not these patients were satisfied with the counseling they received. Others, however, availed themselves of more than one session. A limiting factor for further compilation were the fixed study protocols, with whose help different variables were to be controlled. The intervals between sessions, for example, were sometimes extended due to medical treatments. Therefore, there is only a relatively small sample group whose psychological distress could be measured before as well as after the counseling period. In the study's sample group, no changes occurred over the course of the study period in any patient's condition from the standpoint of their illness. Therefore the question of whether a patient's psychological state could be influenced by a change in acute medical aspects of their condition cannot be addressed. The need for psycho-oncological support specified in the literature is supported despite already proven evidence not in line with those claims. Another study concluded that 1/3 of cancer patients suffered psychiatric comorbidities at the beginning of their acute treatments. The desire for psychosocial support fluctuated according to professional groups [23]. Most frequently, those asked responded that they would like this support to come from their doctor (83%). 77% would have liked this support to come from the caregiving personnel, and only 30% wanted support to come from a psychologist. In the relevant literature, the demand for offers of psycho-oncological support come predominantly from educated, socially secure patients with breast cancer between the ages of 40 and 60. Male patients with other tumor diagnoses, patients with lower social status and elderly people accepted support less often [24]. This conclusion is also confirmed by our findings.
A further point of criticism could be directed at the investigative tools with whose help the effects of a session were to be reflected. Though the instruments were specifically recommended for clinical monitoring and therapeutic evaluation, all the afflictions described in FBK-R23 (for instance, “Anxiety” or “Social Distress”) are difficult to treat. Usually, these topics are treated over a longer counseling period than “Information Deficit”, the topic for which this study found the most improvement.
The findings presented here make possible a first look at the exercise and effectiveness of outpatient psycho-oncological and psycho-social counseling. In order to continue to develop services that meet patients' needs, an understanding of these needs is important. Both psycho-oncological and psychosocial questionnaires are central to the talks. Accordingly, it seems wise to add a second focus: In addition to psycho-oncological skills, developing the psycho-social skills of workers in the counseling center seems a highly worthwhile project. At this point, it is still not clear just how much distress the family members of tumor patients experience, and how this can be effectively operated.
Acknowledgements
This research was made possible by the “Berliner Krebsgesellschaft”. We would also like to thank the patients who so kindly gave of their time to participate in this research.
Conflict of Interest
The authors have declared that no conflict of interest exists.
References
1. Schwarz R. Die Krebspersönlichkeit. Mythos und klinische Realität. 1994
2. Faller H. Krankheitsverarbeitung bei Krebskranken. Göttingen: Verlag für Angewandte Psychologie. 1998
3. Schwarz R, Krauß O. Palliativmedizin - psychologische Therapie. Internist. 2000;7:612-18
4. Holland J. Psycho-Oncology. New York: Oxford University Press. 1998
5. Ernst J, Schröder C, Schwarz R. et al. Informationsbedarf und erwünschte Entscheidungsmitwirkung von Patienten-Empirische Befunde zu soliden und systemischen Krebserkrankungen. Psychoonkologie-Eine Disziplin in der Entwicklung. Koch U, Weis J, editors. Hogrefe: Goettingen Bern Wien Paris Oxford Prag Toronto Cambridge Amsterdam Kopenhagen. 2009
6. Mehnert A, Koch U. Psychosocial care of cancer patients—international differences in definition, healthcare structures, and therapeutic approaches. Supportive Care in Cancer. 2005;13(8):579-88
7. NCCN. Distress management. Clinical practice guidelines. Journal of the National Comprehensive Cancer Network. 2003;1:344-74
8. National Comprehensive Cancer Network. http://www.nccn.org
9. Tschuschke V. Psychoonkologie-Psychologische Aspekte der Entstehung und Bewältigung von Krebs. Stuttgart New York: Schattauer. 2002
10. Keller M. Stand des Wissens zur Wirksamkeit psychosozialer Interventionen. Psychoneuro. 2004;30(04):210-14
11. Fawzy F, Fawzy N, Arndt L. et al. Critical review of psychosocial interventions in cancer care. Archives of General Psychiatry. 1995;52(2):100-13
12. Fawzy FJ. A short-term psychoeducational intervention for patients newly diagnosed with cancer. Supportive Care in Cancer. 1995;3(4):235-38
13. Keller M. Effekte psychosozialer Interventionen auf Lebensqualität und Krankheitsverlauf von Krebspatienten. Der Onkologe. 2001;7(2):133-42
14. Ali N, Khalil H. Effect of psychoeducational intervention on anxiety among Egyptian bladder cancer patients. Cancer Nursing. 1989;12(4):236-42
15. Herschbach P, Marten-Mittag B, Henrich G. Revision und psychometrische Prüfung des Fragebogen zur Belastung von Krebskranken (FBK-R23). Zeitschrift für Medizinische Psychologie. 2003;12(2):69-76
16. Herschbach P, Weis J. Screeningverfahren in der Onkologie. Berlin: Deutsche Krebsgesellschaft eV. 2008
17. Knight L, Mussell M, Brandl T. et al. Development and psychometric evaluation of the Basic Documentation for Psycho-Oncology, a tool for standardized assessment of cancer patients. Journal of Psychosomatic Research. 2008;64(4):373-81
18. Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-74
19. Keller M, Sommerfeldf S, Fischer C. et al. Recognition of distress and psychiatric morbidity in cancer patients: a multi-method approach. Annals of Oncology. 2004;15(8):1243-49
20. Faller H, Olshausen B, Flentje M. Emotional Distress and Needs for Psychosocial Support among Breast Cancer Patients at Start of Radiotherapy. Psychotherapie Psychosomatik Medizinische Psychologie. 2003;53:229-35
21. Loscalzo M. Psychological Issues For The Family. Psycho-oncology. Holland J, ed. Oxford University Press: New York. 1998:981-1032
22. Loscalzo M, Brintzenhofeszoc K. Brief Crisis Counseling. Psycho-oncology. Holland J, ed. Oxford University Press: New York. 1998:662-75
23. Singer S, Bringmann H, Hauss J. et al. Häufigkeit psychischer Begleiterkrankungen und der Wunsch nach psychosozialer Unterstützung bei Tumorpatienten im Akutkrankenhaus. Deutsche Medizinische Wochenschrift. 2007;132(40):2071-76
24. Meyer TJ, Mark MM. Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychology. 1995;14(2):101-8
Author contact
![]() Corresponding author: Ute Goerling, Tel: 0049 30 450 564 623, E-Mail: ute.goerlingde
Corresponding author: Ute Goerling, Tel: 0049 30 450 564 623, E-Mail: ute.goerlingde

 Global reach, higher impact
Global reach, higher impact