Impact Factor
ISSN: 1837-9664
J Cancer 2016; 7(11):1481-1486. doi:10.7150/jca.15466 This issue Cite
Research Paper
Narrowing Resection of Parametrial Tissues Is Feasible in Low-Risk Cases of Stage IA2-IB1 Cervical Cancer
1. Department of Gynecology, OB/GYN Hospital, Fudan University, Shanghai, China;
2. Shanghai Key Laboratory of Female Reproductive Endocrine-Related Diseases, Shanghai, China.
*These authors (Xue-Lian Li, Xiao-Xia Liu) contribute equally to this study and share first authorship. All authors had access to the data and a role in writing the manuscript.
Received 2016-3-6; Accepted 2016-5-24; Published 2016-7-5
Abstract
BACKGROUND: Radical hysterectomy with pelvic lymphadenectomy is the standard surgical treatment for patients with stage IA2-IB1 cervical cancer, but the wide excision increases the complications.
OBJECTIVE: To analyze the feasibility of narrowing resection of parametrial tissues in stage IA2-IB1 cervical cancer.
STUDY DESIGN: Retrospectively analyzed the pathological and clinical data of patients with stage IA2-IB1 cervical cancer who received radical hysterectomy with pelvic lymphadenectomy in OB/GYN Hospital, Fudan University, China from Jan 2008 to Dec 2011. The affected factors of parametrial metastases and outcomes were discussed. The single factor analysis was made with χ2 test, and the relationship of the resection width of parametrial tissues and the patients' outcomes was analyzed with χ2 test and log-rank. P-values <0.05 were considered statistically significant.
RESULTS: There were 31 cases recurred, 26 cases died of cervical cancer in 513 patients during the follow-up period (from 2 months to 66 months, averaged 39 months). The low-risk factors included diameter of tumor ≤2cm, depth of cervical myometrial invasion<1/2 and without lymph vascular involvement. There were no parametrial metastases in cases with all three low-risk factors. Whether the resection width of parametrial tissues ≥3cm or not had no statistically significant effect on progression free survival (PFS) or overall survival (OS) of low-risk patients. D2-40 and CD31 were related with parametrial metastases, but not with recurrence or outcomes.
CONCLUSIONS: The resection width of parametrial tissues has no effect on PFS and OS of low-risk patients, and narrowing resection of parametrial tissues (<3cm) is feasible.
Keywords: stage IA2-IB1 cervical cancer, parametrial metastases, low-risk factors, narrowing resection of parametrial tissues.
Introduction
Cervical cancer is one of the most common cancers of the female reproductive system. The number of women with newly diagnosed cervical cancer increases and the percentage of women with cervical cancer in all gynaecological cancers also increases annually in China[1]. Radical hysterectomy with pelvic lymphadenectomy is the standard surgical treatment for patients with stage IA2-IB1 cervical cancer. But the wide excision of parametrial tissues (≥3cm) increases the complications during and after the operation, especially the complications of the urinary system, which severely affect the life quality and the following adjuvant therapy[2], even in robotic sugeries[3]. Can we decrease the complication by appropriately narrowing the scope of operation in selected patients without affecting the outcomes? How can we choose the proper patients? Therefore, we performed this retrospective analysis and try to answer these questions.
Materials and methods
Data on this retrospective study was collected from The Hospital of Obstetrics & Gynaecology, Shanghai Medical College, Fudan University, Shanghai, China from Jan 2008 to Dec 2011, with the approval of Ethics Committee of hospital. This hospital serves a diverse urban and rural population with over 1.3 million outpatients and 40,000 inpatients annually, and is a largest specialised referral obstetrics & gynaecology teaching hospital located in Shanghai which is the largest city in China with 20 million populations.
The pathological and clinical data of patients with stage IA2-IB1 cervical cancer who received radical hysterectomy with pelvic lymphadenectomy in this OB/GYN Hospital were collected and analyzed. All those patients received either chemotherapy or radiotherapy before the operations were excluded. This retrospective study was exempt from IRB approval because we only reviewed the clinical histories without revolving any information about patients' private.
Immunohistochemical examinations of D2-40 and CD31 were described as negative, positive and strong positive. Strong positive of D2-40 and CD31 meant D2-40 and CD31 positive and also with tumor thrombus.
Those patients with diameter of tumor ≤2cm, depth of cervical myometrial invasion<1/2 and without lymph vascular involvement formed the low-risk group, and the others formed the high-risk group. Both groups were further divided into two groups according to the resection width of parametrial tissues. Those patients with the resection width of parametrial tissues of both sides ≥3cm formed group A, and those with the resection width of parametrial tissues of at least one side <3cm formed group B.
Statistical analysis
The single factor analysis of the pathological and clinical data of patients was made with χ2 test. The relationship of the resection width of parametrial tissues and the patients' outcomes was analyzed with χ2 test and log-rank. P-values <0.05 were considered statistically significant.
Results
There were 880 cases of stage IA2-IB1 cervical cancer received radical hysterectomy with pelvic lymphadenectomy in this hospital from Jan 2008 to Dec 2011. The whole picture of these patients was showed as Table 1. The average age was 45.7±8.7. Among 513 patients with well following-up, there were 31 cases (6.0%) recurred and 26 cases (5.1%) died of cervical cancer during the follow-up period (from 2 months to 66 months, averaged 39 months).
The whole picture of 880 patients with stage IA2-IB1 cervical cancer.
| characteristics | cases (percent,%) |
|---|---|
| pathological type | |
| squamous cell carcinoma | 718 (81.6) |
| adenocarcinoma | 131 (14.9) |
| adenosquamous carcinoma | 19 (2.2) |
| special type | 12 (1.4) |
| NCCN 2014 staging | |
| ⅠA2 | 26 (3.0) |
| ⅠB1 | 854 (97.0) |
| Depth of cervical myometrial invasion | |
| <1/2 | 527 (59.9) |
| ≥1/2 | 353 (40.1) |
| Diameter of tumor | |
| ≤2cm | 513 (58.3) |
| >2cm | 367 (41.7) |
| Lymph vascular involvement | |
| no | 591 (67.2) |
| yes | 289 (32.8) |
| Parametrial metastases | |
| no | 859 (97.6) |
| yes | 21 (2.4) |
| Resection width of parametrial tissues of 513 cases with well following up | |
| Both sides≥3cm | 223 (43.5) |
| At least one side<3cm | 290 (56.5) |
| Immunohistochemical examinations of CD31(542 cases without parametrial metastases) | |
| CD31- | 226 (41.7) |
| CD31+ | 180 (33.2) |
| CD31++ | 136 (25.1) |
| Immunohistochemical examinations of D2-40(585 cases without parametrial metastases) D2-40- | 234 (40.0) |
| D2-40+ | 181 (30.9) |
| D2-40++ | 170 (29.1) |
| Outcomes of 513 cases with well following up | |
| survival recurrence | 456 (88.9) 31 (6.0) |
| death | 26 (5.1) |
The single factor analysis showed that the diameter of tumor was separately related to the depth of cervical myometrial invasion (P=0.000), the diameter of tumor and the depth of cervical myometrial invasion were both related to lymph vascular involvement (P=0.000), the diameter of tumor, the depth of cervical myometrial invasion and lymph vascular involvement were all related to parametrial metastases (P=0.000), shown as Table 2.
Immunohistochemical examinations of D2-40 were applied to 606 cases and examinations of CD31 were applied to 563 cases. CD31 strong positive (P=0.002) and D2-40 strong positive (P=0.016) were also the high-risk factors of parametrial metastases (shown as Table 2).
The relationship of the diameter of tumor, the depth of cervical myometrial invasion, lymph vascular involvement and parametrial metastases.
| Variables (n=880) | Depth of cervical myometrial invasion (cases) | Lymph vascular involvement (cases) | Parametrial metastases (cases) | P value | |||
|---|---|---|---|---|---|---|---|
| <1/2 | ≥1/2 | - | + | - | + | ||
| Diameter of tumor | 0.000* | ||||||
| ≤2cm | 415 | 98 | 406 | 107 | 510 | 3 | 0.000** |
| >2cm | 111 | 256 | 185 | 182 | 349 | 18 | 0.000*** |
| Depth of cervical myometrial invasion | |||||||
| <1/2 | 438 | 89 | 524 | 3 | 0.000# | ||
| ≥1/2 | 153 | 200 | 335 | 18 | 0.000## | ||
| Lymph vascular involvement | |||||||
| - | 587 | 4 | 0.000 | ||||
| + | 272 | 17 | |||||
| CD31 | |||||||
| - | 226 | 3 | 0.320 | ||||
| + | 180 | 6 | |||||
| ++ | 136 | 12 | 0.002 | ||||
| D2-40 | |||||||
| - | 234 | 4 | 0.478 | ||||
| + | 181 | 6 | |||||
| ++ | 170 | 11 | 0.016 | ||||
Note:
* The relationship of the diameter of tumor and the depth of cervical myometrial invasion
** The relationship of the diameter of tumor and lymph vascular involvement
*** The relationship of the diameter of tumor and parametrial metastases
# The relationship of the depth of cervical myometrial invasion and lymph vascular involvement
## The relationship of the depth of cervical myometrial invasion and parametrial metastases.
The χ2 test showed that parametrial metastases were related to the recurrence (P=0.030) and the death (P=0.019) of cervical cancer, but the immunohistochemical indexes were not related to the recurrence or the death of cervical cancer (P>0.05), shown as Table 3.
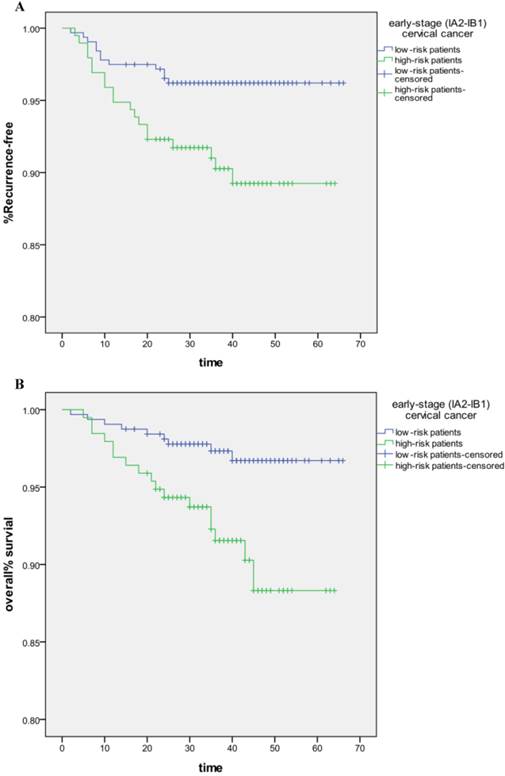
The parametrial metastases rate and transfer rate of high-risk group were 4.1% and 9.5%, while those of low-risk group were 0% and 1.4%, shown as Figure 1. The difference of progression free survival (PFS, P=0.006) and overall survival (OS, P=0.004)) of low-risk and high-risk groups was statistically significant. The resection width of parametrial tissues (varied mostly due to tumor size, performance of different surgeons and the objective conditions of patients) had no statistically significant effect on the recurrence (P=1.000) and the death (P=1.000) of low-risk patients, shown as Table 4. The resection width of parametrial tissues also had no statistically significant effect on the recurrence (P=0.082) and the death (P=0.147) of high-risk patients, shown as Table 4. The resection width of parametrial tissues also had no statistically significant effect on the PFS (P=0.610) and OS (P=0.608) of low-risk patients, shown as Figure 2.
The high-risk factors of recurrence and death of cervical cancer.
| Variables (n=513*) | Recurrence | P | Death | P value | ||
|---|---|---|---|---|---|---|
| No (cases) | Yes (cases) | No (cases) | Yes (cases) | |||
| Parametrial metastases | ||||||
| No | 473 | 28 | 0.030 | 478 | 23 | 0.019 |
| Yes | 9 | 3 | 9 | 3 | ||
| CD31 | ||||||
| - | 123 | 13 | 0.231 | 126 | 9 | 0.712 |
| + | 104 | 6 | 105 | 5 | ||
| ++ | 28 | 7 | 0.156 | 79 | 6 | 0.911 |
| D240 | ||||||
| - | 123 | 13 | 0.119 | 126 | 9 | 0.271 |
| + | 108 | 5 | 109 | 4 | ||
| ++ | 91 | 9 | 0.884 | 92 | 8 | 0.520 |
Note: * 513 cases with well following up.
The relationship of the resection width of parametrial tissues and the recurrence and death of cervical cancer
| Parametrial (cases) | Recurrence | P | Death | P value | ||
|---|---|---|---|---|---|---|
| No (cases) | Yes (cases) | No (cases) | Yes (cases) | |||
| Low-risk group (n=218) | ||||||
| <3cm | 112 | 2 | 1.000 | 112 | 2 | 1.000 |
| ≥3cm | 103 | 1 | 103 | 1 | ||
| High-risk group (n=295) | ||||||
| <3cm | 155 | 21 | 0.082 | 159 | 17 | 0.147 |
| ≥3cm | 112 | 7 | 113 | 6 | ||
Note: This includes 513 cases with well following up.
Discussion
According to the guideline of NCCN 2014, the standard surgical treatment for patients with stage IA2-IB1 cervical cancer is radical hysterectomy with pelvic lymphadenectomy, which demands wide excision of parametrial tissues (cardinal ligament 3-4cm, uterosacral ligament≥3cm and all vaginal connective tissues). The wide excision of parametrial tissues may block pelvic nerves which locate in cardinal ligament and uterosacral ligament, and increase the complications during and after the operation, especially the complications of the urinary system, which may severely affect the life quality and the following adjuvant therapy [2,3]. Studies of large samples have shown that the parametrial metastases rate of stage 1B1 cervical cancer is about 5.4-10% [4-5]. The parametrial metastases rate of those patients with the diameter of tumor ≤2cm, the depth of cervical myometrial invasion<10 mm and without lymph vascular involvement is about 0-1.1% [4-6], which suggest that these factors can be considered as low-risk factors. On the other hand, there was a report of 37 patients with stage 1A2-1B1 cervical cancer showing that the parametrial metastases rate was 33% for all patients and 4.5% for those with the diameter of tumor ≤2cm and without lymph vascular involvement[7], but this result should be doubted because of the limited cases and the miss of considering the depth of cervical myometrial invasion.
In our study, 880 patients with stage IA2-IB1 cervical cancer were analyzed and the total parametrial metastases rate was 2.4%. The single factor analysis showed that the diameter of tumor >2cm, the depth of cervical myometrial invasion ≥1/2 and lymph vascular involvement were all independent high-risk factors of parametrial metastases. There were no parametrial metastases in cases with the diameter of tumor ≤2cm, the depth of cervical myometrial invasion<1/2 and without lymph vascular involvement at the same time, which suggested that over resection of parametrial tissues was not wise for these low-risk patients. Can we narrow the range of operation, decrease the possible complications and improve the life quality while without bad effect on the outcomes of these low-risk patients? The feasibility and safety of narrowing the scope of operation in selected patients are worthy of further discussion.
The differences of PFS and OS of high-risk and low-risk group. A. The differences of PFS (P=0.006). B. The differences of OS (P=0.004).
The effect of the resection width of parametrial tissues on PFS (A, P=0.610) and OS (B, P=0.608) of low-risk patients.
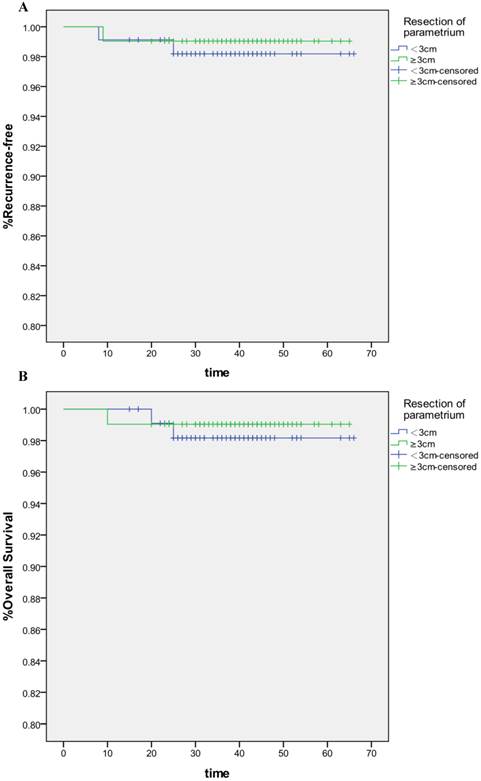
Among cases of stage IA2-IB1 cervical cancer which should have received radical hysterectomy with pelvic lymphadenectomy according to the guideline of NCCN 2014, there were 290 (56.5%) cases whose actual resection width of parametrial tissues of at least one side <3cm, which is mostly varied mostly due to tumor size, performance of surgeons and the objective conditions of patients. We analyzed these cases and found out that the recurrence rate was 1.4% for low-risk patients, which was lower than 9.5% for other patients. Among all low-risk patients, the recurrence rate of those with the resection width of parametrial tissues of at least one side <3cm (group B) was 1.8%, which had no statistically difference with that (0.1%) of patients with the resection width of parametrial tissues of both sides ≥3cm (group A). Among all high-risk patients, the recurrence rate of group B was 13.5% and also had no statistically difference with that of group A (6.3%), which may be due to the adjuvant chemotherapy, radiotherapy or both after the operation. The PFS and OS of high-risk patients, even with the help of adjuvant chemotherapy, radiotherapy or both after the operation, were still lower than those of low-risk patients. The resection width of parametrial tissues had no statistically significant effect on the PFS and OS of low-risk patients and further supported the feasibility and safety of narrowing the range of operation in low-risk patients, which was also supported by another paper [8].
But how can we accurately value those patients of cervical cancer before operation since the staging of cervical cancer is based on clinical characteristics? How can we exclude the high-risk factors? The magnetic resonance imaging (MRI) and pelvic reconstruction can help with the accurate assessment of the diameter of tumor and the depth of cervical myometrial invasion. So the accurate assessment of lymph vascular involvement becomes a key point of excluding the high-risk factors before operation.
The D2-40 antibody plays an important role in routine histopathologic diagnostics of normal lymphatic vessels and lymphaticderived tumors [9]. Platelet/endothelial cell adhesion molecule-1 (CD31) is a cell adhesion and signaling molecule which plays in the biology of blood and vascular cells [10]. So we used strong positive of D2-40 to stand by the lymphatic vessel invasion and strong positive of CD31 to stand by the vascular invasion of cervical cancer, and found out that strong positive of D2-40 and CD31 may suggest the parametrial metastases, although the expressive level of CD31 and D2-40 had no relationship with the recurrence and death of cervical cancer. So we can make a fairly precise assessment of whether there is lymph vascular involvement or not by immunohistochemical examination of the expressive level of CD31 and D2-40 in the specimens of cervical biopsy or loop electrosurgical excision procedure of patients with cervical cancer.
There are some limitations to this study. The expression status of D2-40 and CD31 were not represented by the density of the lymphatic ducts and blood vessels. Due to the length of the study and the number of cases included, it was difficult to suggest the exact size of narrowing resection of parametrial tissues which is feasible and safe for low-risk patients.
In summary, this retrospective analysis has shown that the diameter of tumor >2cm, the depth of cervical myometrial invasion ≥1/2 and lymph vascular involvement are all independent high-risk factors of parametrial metastases, and further highly related to the outcomes of stage IA2-IB1 cervical cancer. Low-risk patients without any of these three high-risk factors have fairly optimistic outcomes, and narrowing the range of operation, which means narrowing resection of parametrial tissues (<3cm), is feasible and safe for low-risk patients. MRI, combined with the immunohistochemical examination of D2-40 and CD31, can help with excluding the high-risk factors before operation.
Acknowledgements
This study was supported by National Natural Science Foundation of China (grant No.31371452 to Hua Jiang) and Foundation from Science and Technology Commission of Shanghai Municipality (grant No.15JC1403202 to Hua Jiang).
Competing Interests
None of the authors have a conflict interest.
References
1. Li X, Zheng S, Chen S. et al. Trends in gynaecological cancers in the largest obstetrics and gynaecology hospital in China from 2003 to 2013. Tumor Biol. 2015;36(7):4961-6
2. Ware RA, van Nagell JR. Radical Hysterectomy with Pelvic Lymphadenectomy: Indications, Technique, and Complications. Obstet Gynecol Int. 2010;2010:587610
3. Hao X, Han S, Wang Y. Comparison of conventional laparoscopy and robotic radical hysterectomy for early-stage cervical cancer: A meta-analysis. J Cancer Res Ther. 2015;11:258-64
4. Kodama J, Kusumoto T, Nakamura K. et al. Factors associated with parametrial involvement in stage IB1 cervical cancer and identification of patients suitable for less radical surgery. Gynecol Oncol. 2011;122(3):491-4
5. Chang S J, Bristow R E, Ryu H S. A model for prediction of parametrial involvement and feasibility of less radical resection of parametrium in patients with FIGO stage IB1 cervical cancer. Gynecol Oncol. 2012;126(1):82-6
6. Klat J, Sevcik L, Simetka O. et al. What is the risk for parametrial involvement in women with early-stage cervical cancer with tumour <20 mm and with negative sentinel lymph nodes? Aust N Z J Obstet Gynaecol. 2012;52(6):540-4
7. Coutant C, Cordier AG, Guillo E. et al. Clues pointing to simple hysterectomy to treat early-stage cervical cancer. Oncol Rep. 2009;22(4):927-34
8. Cai HB, Chen HZ, Zhou YF. et al. Class II radical hysterectomy in low-risk IB squamous cell carcinoma of cervix: a safe and effective option. Int J Gynecol Cancer. 2009;19(1):46-9
9. Szolkowska M, Langfort R, Winiarski S. et al. D2-40 Antibody is a Specific Marker for B2 Thymomas. Appl Immunohistochem Mol Morphol. 2016 [Epub ahead of print]
10. Lertkiatmongkol P, Liao D, Mei H. et al. Endothelial functions of platelet/endothelial cell adhesion molecule-1 (CD31). Curr Opin Hematol. 2016;23(3):253-9
Author contact
![]() Corresponding author: Hua Jiang, OB&GYN Hospital of Fudan University, 419 Fang-Xie Road, Shanghai 200011, China. E-mail address: jianghuaedu.cn. Fax: +86 21 63455090.
Corresponding author: Hua Jiang, OB&GYN Hospital of Fudan University, 419 Fang-Xie Road, Shanghai 200011, China. E-mail address: jianghuaedu.cn. Fax: +86 21 63455090.

 Global reach, higher impact
Global reach, higher impact