Impact Factor
ISSN: 1837-9664
J Cancer 2021; 12(12):3701-3714. doi:10.7150/jca.58580 This issue Cite
Research Paper
Prospective Non-Randomized Study of Intraoperative Assessment of Surgical Resection Margin of Colo-Rectal Liver Metastases
1. Clinic for Surgical Oncology, Oncology Institute of Vojvodina, Sremska Kamenica, Serbia.
2. Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia.
3. Armed Forces of Bosnia and Herzegovina, Logistics Command, Doboj, Bosnia and Herzegovina.
4. Department of Pathoanatomical and Laboratory Diagnostics, Oncology Institute of Vojvodina, Sremska Kamenica, Serbia.
5. Clinic for Internal Oncology, Oncology Institute of Vojvodina, Sremska Kamenica, Serbia.
6. Department of Pathology, Hackensack University Medical Center, Hackensack, New Jersey, USA.
7. Department of Pathology, Hackensack Meridian School of Medicine, Nutley, New Jersey, USA.
8. Uniformed Services University of the Health Sciences, Bethesda, Maryland, USA.
* contributed equally to this study and will share first authorship.
Abstract
Introduction: More than 50% of patients with colorectal cancer (CRC) develop liver metastases during the natural course of disease. Surgical resection is currently the most potentially curative method in the treatment of colorectal liver metastases (CRLM). The goal of surgery is to achieve a negative resection margin (RM) of at least 1 mm, which provides the best prognosis for patients. The RM can be assessed by the pathologist of the resected liver specimen (RLS) and by the surgeon intraoperatively. The aim of this research paper is to determine the degree of agreement on intraoperative assessment of the RM by the surgeon and histopathological RM assessment by the pathologist.
Material and methods: This prospective non-randomized double-blind study was approved by the Ethics Committee of the Oncology Institute of Vojvodina and registered on ClinicalTrials.gov #NCT04634526. The study was conducted at the Oncology Institute of Vojvodina, Sremska Kamenica, Serbia. An experienced hepatobiliary surgeon assessed RM for every specimen intra-operatively, immediately after CRLM resection. Resected CRLM lesions were analyzed by two experienced pathologists. These data were compared with pathological RM assessment as a “gold standard”. RM of 1 mm or more was rated as negative RM (RM-). Disease-free survival (DFS) and recurrence rate was calculated by RM status defined by surgeon and by pathologist.
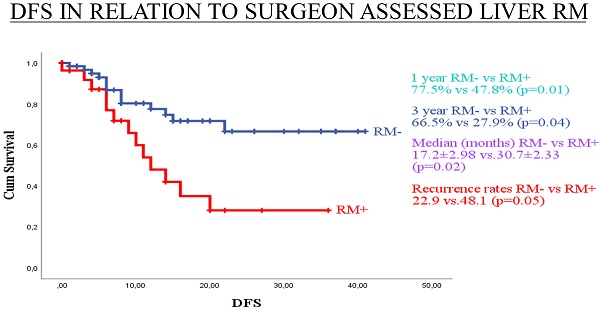
Results: From 01 January 2015 to 31 August 2019, 98 patients were enrolled in the study. There were 219 RLS with 245 CRLM. The surgeon registered positive RM (RM+) of <1mm in 41 (18.7%) RLS. Taking the result of the histopathological assessment (HPA) as the “gold standard”, it was determined that RM was true positive in 32 (14.6%) cases. False positive RM was found in 9 (4.1%) cases. False negative RM was found in 20 (9.1%) cases. True negative RM was found in 158 (72.2%) cases. Sensitivity of surgical assessment (SA) of RM+ was 61.5% (32/52). Specificity of SA of RM+ was 94.6% (158/167). The positive predictive value (PPV) was 78.0% (32/41), while the negative predictive value (NPV) was 88.8% (158/178). The overall accuracy of the RM+ SA was 86.8% (190/219). There was no statistically significant difference in the assessment of RM+ per RLS by surgeon and pathologists (p=0.061), but it was significant when analyses per patients was performed (p=0.017). Recurrence rate for RM+ patients was 48.1% (13/27, p=0.05) for SA and 35.0% (14/40, p=0.17) for HPA. Three year DFS for RM- and RM+ was 66.5% and 27.9% (p=0.04), respectively, by SA, and 64.8% and 42.1% (p=0.106), respectively, by HPA.
Conclusion: Intraoperative assessment of RM- by surgeon of RLS is clinically meaningful. There is not a statistically significant difference in the assessment of RM+ by surgeon and pathologists per RLS, but it was statically significant on a per patient basis. RM determined by surgeon has better prognostic impact on recurrence rate and 1- and 3-year DFS than standard histopathological assessment.
Keywords: colon cancer, liver metastases, resection, resection margin, recurrence, disease-free survival

 Global reach, higher impact
Global reach, higher impact