3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2021; 12(19):5848-5863. doi:10.7150/jca.60152 This issue Cite
Research Paper
Extranodal Extension in Bilateral Cervical Metastases: A predictor of Undesirable Survival Outcomes despite Aggressive Salvage Treatment in Oral Cancer Patients
1. Department of Dermatology, Huashan Hospital affiliated by Fudan University, No.12, Wulumuqi Middle Road, Shanghai, China.
2. Department of Maxillofacial - Head & Neck Oncology, 9th People's Hospital, Shanghai Jiao Tong University School of Medicine, National Research Center for Oral Diseases, Shanghai Key Laboratory of Stomatology, No. 639, Zhi Zao Ju Road, Shanghai 200011, China.
3. Department of Oral Pathology, 9th People's Hospital, Shanghai Jiao Tong University School of Medicine, No. 639, Zhi Zao Ju Road, Shanghai 200011, China.
4. Department of Radiology, 9th People's Hospital, Shanghai Jiao Tong University School of Medicine, No. 639, Zhi Zao Ju Road, Shanghai 200011, China.
5. Department of Oral and Maxillofacial Surgery, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang, China.
*Co-first authors with equal contributions to this manuscript.
Abstract
Objectives: Despite the inclusion of extranodal extension (ENE) in the recent staging system, the presence of ENE alone is not sufficient to depict all clinical situations, as ENE is frequently found in multiple nodes. Thus, the purpose of this study was to evaluate the surgery-based treatment outcomes and clinicopathological features of oral cavity squamous cell carcinoma (OCSCC) patients with ENE found in bilateral multiple cervical metastases.
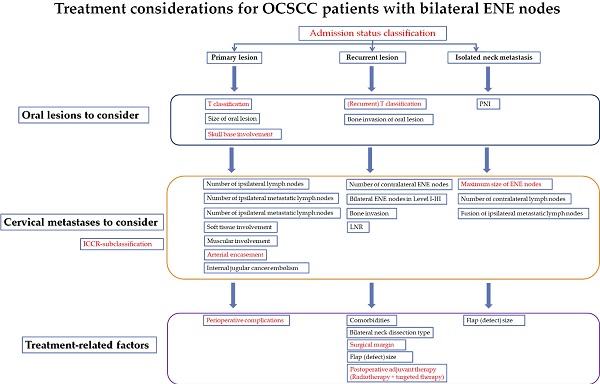
Materials and methods: A retrospective single-institutional study of OCSCC patients with bilateral ENE nodes was performed from January 2011 to December 2018. OCSCC patients of different admission statuses (with primary lesions (PL), recurrent lesions (RL) and isolated neck metastases (INM)) were included for subgroup comparisons. All patients received surgical treatment with/without adjuvant therapies and had complete follow-up data. Disease-free survival (DFS) was regarded as the main outcome. Time-to-relapse data were also collected for comparison.
Results: A total of 128 patients were included, of whom 97 (75.8%) were male. The mean follow-up period reached 15 months. Among the patients, 85 (66.4%) were treated for PLs, followed by 26 (20.3%) treated for RLs after failed prior therapy and 17 (13.3%) treated for INMs (concurrent or sequential). The DFS rate was merely 35.2%. Treatment-related factors such as surgical margin (p=0.003), postoperative adjuvant therapy (p=0.014) and perioperative complications (p=0.036) were significantly associated with patient outcomes. In addition, oral lesion-related variables such as oral subsites (p=0.037), T classification (p=0.026) and skull base involvement (p=0.040) were indicators of a worse prognosis. For bilateral ENE features, ENE subclassification (p=0.036), maximum size of ENE nodes (p=0.039) and arterial nodal encasement (p=0.025) tended to predict the surgery-based treatment outcomes of these patients.
Conclusions: Bilateral cervical metastases with ENE features, though uncommon, are a serious regional burden, and these patients have lower-than-expected treatment outcomes, especially those with RLs or INMs. A fairly large number of OCSCC patients with advanced oral lesions gain little benefit from intensified salvage surgical treatment. Such treatment should instead be offered to select patients with smaller bilateral ENE nodes (<3 cm) and those with lower ENE subclassifications and no arterial nodal encasement.
Keywords: bilateral, extranodal extension, cervical metastasis, oral cancer, surgery, survival

 Global reach, higher impact
Global reach, higher impact