3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2021; 12(19):5923-5928. doi:10.7150/jca.62090 This issue Cite
Research Paper
Preoperative LMR and Serum CA125 Level as Risk Factors for Advanced Stage of Ovarian Cancer
1. Department of Obstetrics and Gynecology, The Affiliated Nanchong Central Hospital of North Sichuan Medical College, Nanchong, Sichuan, China.
2. North Sichuan Medical College, Nanchong, Sichuan, China.
#These authors contributed equally to this work.
Abstract
Objectives: This study was to analyze the relationships between lymphocyte-to-monocyte ratio (LMR) alone or combined with serum CA125 (COLC) and advanced stage of ovarian cancer (OC).
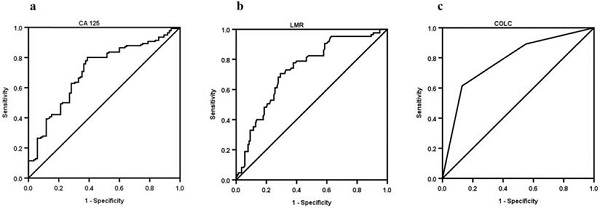
Methods: The receiver-operating characteristic (ROC) curves of LMR, CA125, and COLC staging OC were constructed by a retrospective study. Furthermore, a binary logistic regression model was used to assay the independent risk factors for OC staging.
Results: Two hundred and twenty-five patients with OC were identified in this cohort. Eighty-five OC patients were diagnosed at an early stage, and 140 OC patients were diagnosed at an advanced stage. The median of LMR in the early stage was higher than that in advanced stage (4.4 vs. 2.8), and the median of serum CA125 was lower than that in advanced stage (80 U/mL vs. 251.3 U/mL). Multivariate logistic regression LMR≤3.7 (OR=0.299, 95% CI: 0.093-0.962, P=0.043) and CA125>95.7 U/mL (OR=4.317, 95% CI: 1.436-12.977, P=0.009) were risk factors for stage of advanced OC whether presence or absence of malignant ascites. Furthermore, the area under the curve of COLC was higher than that of LMR (0.782 vs. 0.732) or serum CA125 (0.782 vs. 0.708) in staging OC. The specificity of COLC was higher than that of LMR (87.1% vs. 70.6%) or serum CA125 (87.1% vs. 61.2%) in staging OC.
Conclusion: LMR alone or in combination with serum CA125 might be associated with OC staging. Besides, as a predictive factor, COLC may have a high specificity in staging OC.
Keywords: Ovarian cancer, lymphocyte-to-monocyte ratio (LMR), CA125, International Federation of Gynecology and Obstetrics (FIGO), stage, combine

 Global reach, higher impact
Global reach, higher impact