3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2022; 13(14):3575-3583. doi:10.7150/jca.78009 This issue Cite
Research Paper
Patterns of lymph node metastases and their implications in individualized radiotherapeutic clinical target volume delineation of regional lymph nodes in patients with endometrial cancer
1. Department of Gynecology and Obstetrics, Tianjin Medical University General Hospital, Tianjin, China.
2. Tianjin Key Laboratory of Female Reproductive Health and Eugenics, Tianjin Medical University General Hospital, Tianjin, China.
3. Department of Pharmacy, Tianjin Medical University General Hospital, Tianjin, China.
*These authors contributed equally to this work.
Abstract
Purpose: To study the patterns of lymph node metastasis (LNM) of endometrial cancer (EC) and to clarify the individualized clinical target volume delineations of regional lymph nodes (CTVn).
Methods: Data from a total of 556 patients with EC who had undergone total hysterectomy associated with bilateral salpingo-oophorectomy (TH/BSO) and systematic lymphadenectomy were retrospectively examined. The clinicopathological factors related to LNM were analyzed using logistic regression analysis.
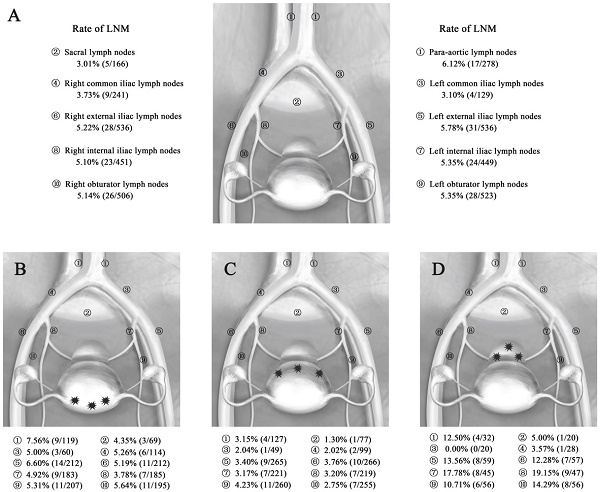
Results: LNM was found in 76 of 556 patients, resulting in a metastasis rate of 13.67%. The rates of LNM in patients with fundus and cornua lesions were 7.56% for para-aortic nodes and 14.41% for pelvic lymph nodes. The rates of LNM in patients with sidewall lesions were 3.15% for para-aortic nodes and 10.22% for pelvic lymph nodes. The rates of LNM in patients with lower uterine segment and cervix lesions were 12.50% for para-aortic nodes and 26.67% for pelvic lymph nodes. Deep myometrial invasion, histological type, histological differentiation, and lymphovascular space invasion (LVSI) emerged as statistically significant risk factors for pelvic LNM of EC (P = 0.008, 0.015, < 0.001, 0.005, respectively). Grade 3 differentiation had a strong influence on LNM to the para-aortic nodes (P = 0.015).
Conclusions: Myometrial invasion, histological type, histological differentiation, and LVSI were related to pelvic LNM and grade 3 was associated with para-aortic LNM. These factors should be considered comprehensively to design the CTVn for intensity-modulated radiation therapy (IMRT) of EC. For patients with lower uterine segment/cervix and fundus/cornua lesions, delineating the irradiation field of the para-aortic nodal region may confer a benefit.
Keywords: Endometrial cancer, Lymph node metastasis, Radiotherapy, Clinical target volume

 Global reach, higher impact
Global reach, higher impact