3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(6):895-902. doi:10.7150/jca.82801 This issue Cite
Research Paper
The effect of radiotherapy time and dose on acute hematologic toxicity during concurrent postoperative chemoradiotherapy for early high-risk cervical cancer
Department of Radiation Oncology, Shanghai Sixth People's Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
Abstract
Objective: This study aims to analyze the characteristics and factors that influence acute hematological toxicity (HT) during concurrent chemoradiotherapy (CCRT) for cervical cancer, as well as to provide reference data for clinical practice.
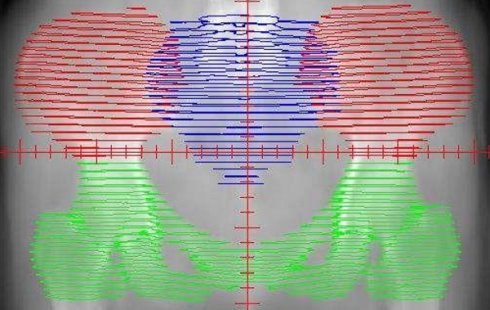
Methods: Patients with FIGO IB1-IIA2 cervical cancer who underwent CCRT from May 2018 to August 2020 were included in this study retrospectively. All patients had received external beam radiation therapy and platinum-based concurrent chemotherapy. HT was assessed according to CTCAE 5.0. The pelvic bone marrow was redrawn on the original CT images and divided into four parts: the whole pelvic bone marrow (WP-BM), iliac bone marrow (IL-BM), lower pelvic bone marrow (LP-BM), and lumbosacral bone marrow (LS-BM). The radiation dose and volume of each part of the pelvic bone marrow were recalculated in a new plan created using the original planning parameters. The corresponding dose-volume histogram (DVH) was generated to obtain the bone marrow volumes receiving 10Gy, 20Gy, 30Gy, 40Gy, 45Gy, and 50Gy.
Results: In 112 patients, the incidences of grade 2 or higher leukopenia, anemia, thrombocytopenia, and neutropenia were 49.1%, 2.7%, 1.8%, and 20.5%, respectively. Leukopenia was linked to LS-V20 (r = -0.310; P = 0.006) and radiotherapy treatment lengths (days) (r = -0.416; P = 0.013). Anemia was associated with WP-V30, WP-V40, WP-V45, WP-V50, IL-V20, IL-V40, ILV45, IL-V50, LP-V30, LP-V40, LP-V45, and LP-V50 (P <0.05). Thrombocytopenia (r = -0.304, P = 0.007) and neutropenia (r = -0.368, P = 0.009) was associated only with the length of radiotherapy treatment (day). Multiple regression analysis showed that only anemia was negatively correlated with WP-V30, IL-V40, and LP-V40 (P <0.05).
Conclusions: Acute HT during CCRT in early-stage high-risk cervical cancer may be related to the duration of radiotherapy and the volume of different radiotherapy doses received at different parts in the pelvic bone marrow.
Keywords: Early-stage high-risk cervical cancer, Concurrent chemoradiotherapy, Acute hematological toxicity, Pelvic bone marrow dose volume

 Global reach, higher impact
Global reach, higher impact