Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(10):1935-1945. doi:10.7150/jca.83162 This issue Cite
Research Paper
Cancer trends and risk factors in China over the past 30 years (1990-2019)
1. Department of Neurology, Union Hospital, Fujian Medical University, Fuzhou, China.
2. Shengli Clinical Medical College of Fujian Medical University, Fuzhou, 350001, China.
3. Department of Urology, Fujian Provincial Hospital, Fuzhou, 350001, Fujian, China.
4. Department of Urology, Juntendo University School of Medicine, Tokyo, Japan.
5. College of Biological Science and Engineering, Fuzhou University, Fuzhou 350108, China.
Received 2023-2-2; Accepted 2023-6-18; Published 2023-6-26
Abstract
Objective: We retrospectively studied cancer mortality and incidence in China from 1990 to 2019, investigated the cancer trends and risk factors, and analyzed the effects of Gross Domestic Product (GDP) on cancer mortality and incidence.
Methods: Data was obtained in "Our world in data" in October 2022 to explore mortality rates of different cancers and their trends and the roles of cancer risk factors, including GDP, air pollution, etc.
Results: Over the past 30 years, cancer had been China's second leading cause of death. Tracheal, bronchial, and lung cancers, with an annual growth rate of 6.5%, were the most frequently diagnosed cancers. The burden of different cancers changed as the mortality rate of cancer changed. The age-standardized cancer mortality rate had decreased by 19.0%; cancer deaths in all age groups had increased. While the number of cancer deaths in the elderly aged ≥70 did not increase distinctively, its percentage increased by 52.1% and 1.7% annually. The percentage of patients with new-onset cancer increased by 240% and 8.6% annually. For every USD 1,000 increase in GDP, cancer deaths decreased by 2.3/100,000. Tobacco, meat, and alcohol consumption and BMI had increased and were not conducive to the future control of cancer.
Conclusions: We summarized the incidence and mortality of major cancers and their trends in China over the past 30 years and analyzed the effects of GDP and the roles of cancer risk factors. Overall GDP growth and effective control of air pollution reduced cancer mortality, while population aging, smoking, alcohol consumption, BMI increasing, and meat consumption brought challenges for cancer control.
Keywords: Cancer trends, risk factor, China, cancer mortality, cancer control, GDP
Introduction
Cancer is one of the leading causes of death in China [1]. As the population ages, changes in cancer risk factors, particularly diet, obesity, diabetes, and air pollution, have led to a shift in the approaches of the Chinese government to cancer control. Although many achievements have been made, challenges have remained [2]. Lung cancer is currently the leading cause of cancer-related deaths in China. Although the burden of upper gastrointestinal cancer is decreasing, the burden of colorectal, prostate, and breast cancers is increasing annually [2]. In terms of gender differences, gastrointestinal cancers, including gastric, colorectal, liver, and esophageal cancers, cause a large cancer burden in both men and women, while breast cancer is the most common type of cancer in women [3]. Lung cancer consistently had the highest mortality and morbidity among men, while prostate cancer had the second highest age-standardized incidence rate among men, increasing by 112% from 1990 to 2017 [4]. The cancer spectrum in China was changing; in addition to the high incidence and burden of liver, stomach, esophagus, and cervical cancers, the incidence and burden of other cancers (lung, breast, colorectal, and prostate) were also rapidly increasing. China's cancer spectrum shifted from developing to developed countries [5]. However, these dynamic change data reports have been relatively limited over the last 30 years and deserve further exploration.
Population-based cancer registries have been operational in China for approximately 60 years; they are a crucial component of China's health priorities, which are also responsible for progress tracking in cancer control [6]. Healthy China 2030 paints a bright vision for the future of cancer control in China [7]. However, reducing the cancer burden in China requires cross-sectoral collaborative and coordinated efforts by the government, public health organizations, and individuals in primary and secondary prevention, and the situation does not appear to be optimistic [2,8]. The purpose of this study was to retrospectively study the trends in cancer incidence and mortality in China over the past 30 years (from 1990 to 2019) and to examine the recognized risk factors for cancer in cancer control, including smoking, alcohol consumption, meat consumption, air pollution, BMI, and gross domestic product (GDP), to provide data support for strategies to achieve China's 2030 Cancer Control Plan.
Method
We obtained permission to attain data on cancer and lifestyle habits in China from "Our world in data" (https://ourworldindata.org/) in October 2022 [9]. This database is intended to address major issues occurring around the world, including major public concerns about cardiovascular diseases, cancer, air pollution, water pollution, dietary hygiene, and the recent coronavirus disease 2019 (COVID-19) pandemic [10]. This database is fully accessible, and the data owners confirmed that we could use, reproduce, and distribute it in any medium as long as the source and its authors were cited accordingly. Therefore, we collected data on all mortality rates in annual units in China from 1990 to 2019 and plotted the trend curves of various causes of death over time. We then focused on the mortality rates and trends of different cancer types to explore age-related mortality rates for different cancers and their trend curves, analyze age-based cancer incidence and its trends, and explore the cancer burden in China over this period. Comparing the percentage of cancer deaths over time with a baseline of 1990, the cancer death rate included both unstandardized and age-standardized cancer death rates. We explored the proportion of non-genetic factors contributing to cancer death in different cancer types, including a wide range of non-genetic external environmental factors such as exposure to carcinogens, GDP, environment, smoking, alcohol consumption, meat consumption, and BMI, which are related to cancer occurrence and death, to provide data reference for reducing cancer deaths in China. All data are presented as numbers and percentages.
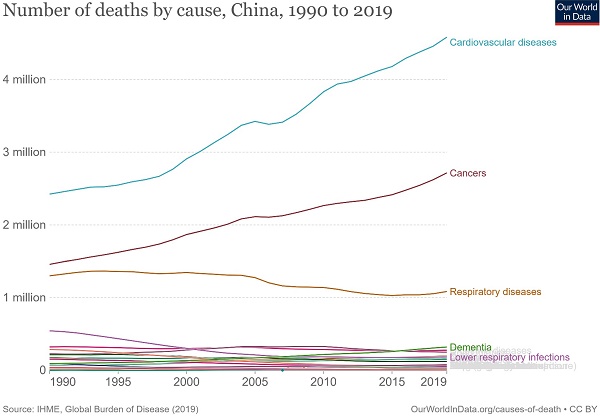
The number and trends of deaths by causes in China from 1990 to 2019.
Results
Cancer mortality and its trends
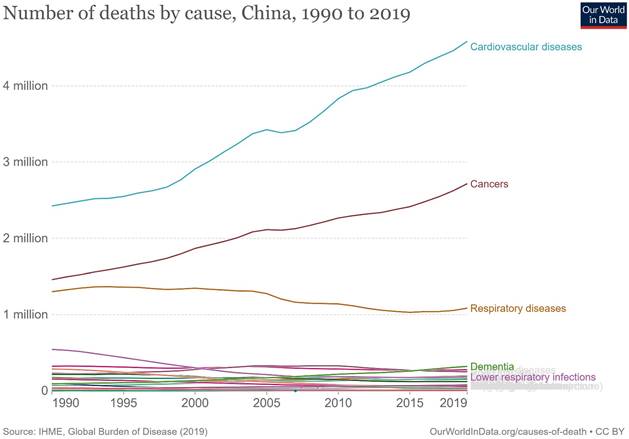
Cancer deaths in China increased from 1.46 million to 2.72 million in 2019, second only to cardiovascular diseases at 4.58 million and 1.63 million more than the third-ranked respiratory diseases (Figure 1). In 1990, the top five cancer deaths were stomach cancer (n = 305,467); tracheal, bronchial, and lung cancer (n = 256,326); liver cancer (n = 232,449); esophageal cancer (n = 176,602); and colon and rectum cancer (n = 79,322). By 2019, the number of cancer deaths had changed, ranking first as tracheal, bronchial, and lung cancers (n = 757,171), with an increase of 195.4% and 6.5% annually. This was followed by stomach cancer (n = 421,539, an increase of 37.9% in total and 1.3% annually), colon and rectal cancer (n = 261,777, an increase of 230.0% in total and 7.7% annually), esophageal cancer (n = 257,316, an increase of 45.7% and 1.5% annually), and liver cancer (n = 187,700, a decrease of 19.3% in total and 0.6% annually). The subsequent fastest-growing cancers were panic cancer (ranked 6th in 2019) and breast cancer (ranked 7th in 2019), which increased by 333.1% and 130.4%, respectively, in 30 years, with respective annual growth rates of 11.1% and 4.3% (Figure 2, Supplemental Figure 1).
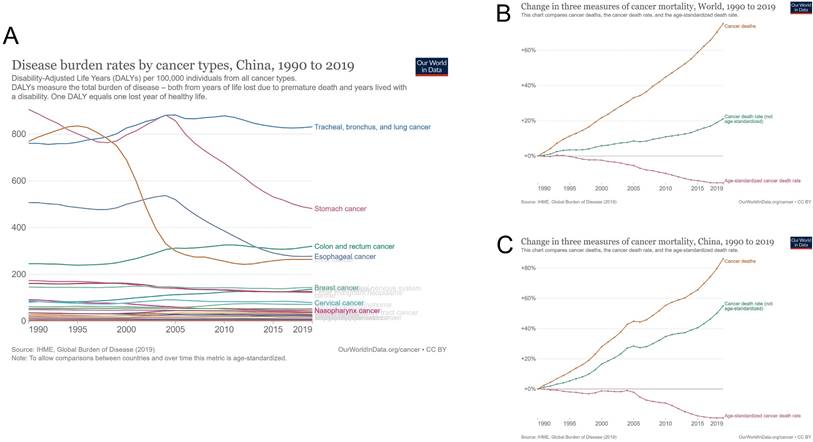
The cancer burden in China has also changed over the past 30 years, and the trend has changed according to cancer mortality. The maximum cancer burden was caused by gastric cancer in 1990, which changed to tracheal, bronchial, and lung cancers in 2019. Among the top five cancers, both esophageal and liver cancer burdens decreased, while colon and rectal cancer burdens steadily increased yearly (Figure 3A). As a result, the cancer mortality rate in China has increased yearly since 1990. By 2019, the cancer mortality rate in China had increased by 86.2%, and the age-unstandardized cancer mortality rate had increased by 54.9%. In contrast, the age-standardized cancer mortality rate dropped significantly (19.0%) in 2019, compared with 1990. Compared with the world cancer mortality rate, China's cancer mortality rate increased more over the past 30 years (world cancer mortality rate increased by 75.1%); however, China's age-standardized cancer mortality rate decreased more evidently (world age-standardized cancer mortality rate decreased by 15.2%) (Figure 3B and 3C).
Cancer deaths by types in China from 1990 to 2019.
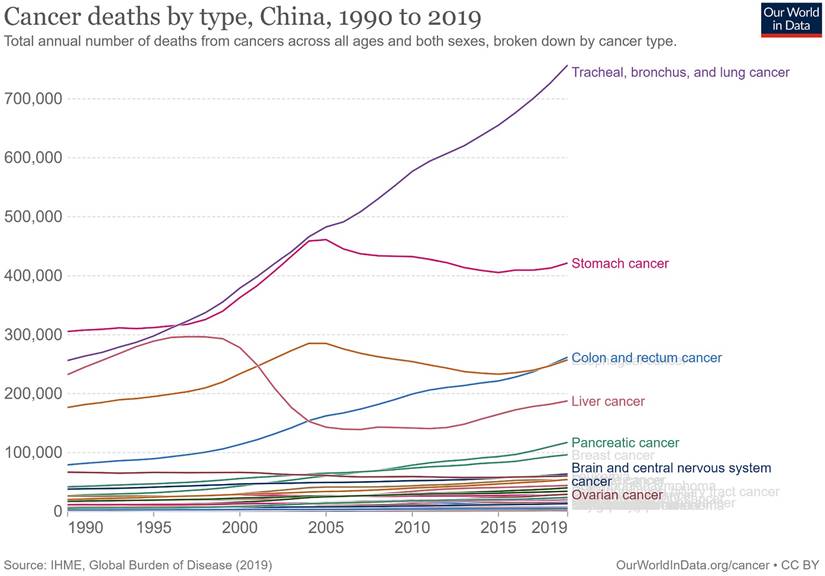
Cancer burden in China from 1990 to 2019. (A) Disease burden rates by cancer types; (B) changes in three measures of cancer mortality in the world from 1990 to 2019; (C) changes in three measures of cancer mortality in China from 1990 to 2019.
Cancer death by age in China from 1990 to 2019. (A) Cancer death rates by age groups; (B) percentage of cancer deaths among age groups.
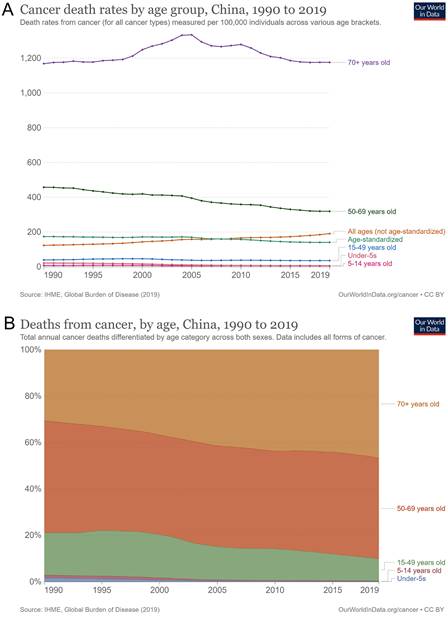
Age-related cancer mortality and trends
Cancer mortality rates in different age groups have changed annually. The number of cancer deaths in all age groups increased from 123.3/100,000 in 1990 to 190.9/100,000 in 2019, an increase of 54.9% in total and 1.8% annually. However, the rate of age-standardized cancer mortality showed a downward trend, a decrease of 19.0% in total and 0.6% annually. Cancer deaths in the elderly aged ≥ 70 years first increased (1334.5/100,000 in 2005) and then decreased, and the increase was not apparent until 2019 (Figure 4A). As a result, the percentage of cancer deaths in the elderly aged ≥ 70 years increased from 30.7% in 1990 to 46.7% in 2019, an increase of 52.1% in total and 1.7% annually. Cancer deaths in people aged 50-69 years had decreased from 457.5/100,000 to 319.1/100,000, a decrease of 30.3% in total and 1.0% annually. The percentage of people aged 50-69 also dropped from 18.1% in 1990 to 9.5%, a decrease of 47.5% in total and 1.6% annually. The numbers of other age groups did not increase; however, their percentages decreased across all age groups (Figure 4B).
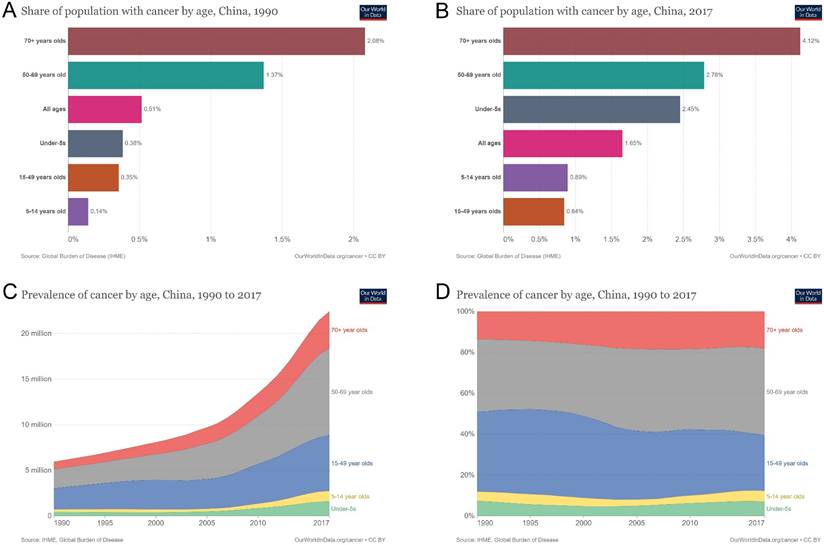
Prevalence of age-related cancer incidence
Cancer incidence in different age groups increased from 0.5% of the population in 1990 to 1.7% in 2017. The percentage of patients with new-onset cancer in the population increased by 240% and 8.6% annually (Figures 5A and 5B). The number of patients with new-onset cancer aged ≥ 70 years was 0.8 million in 1990 and 4.1 million in 2017, an increase of 412.5% in total and 14.7% annually. The number of patients aged 50-69 years increased from 2.1 to 9.53 million, an increase of 353.8% and 12.6% annually. The number of patients aged 15-49 increased from 2.3 million to 6.1 million, 165.2% in total and 5.9% annually (Figure 5C). Among the proportions of patients of different ages, the proportion of patients with new-onset cancer aged ≥ 70 years increased from 13.6% to 18.1%, a growth rate of 33.1% in total and 1.2% annually. The proportion of patients with new-onset cancer aged 50-69 increased from 35.5% to 42.5%, a growth rate of 19.7% in total and 0.7% annually. For patients with new-onset cancer aged 15-49 years, the percentage decreased from 39.1% to 27.2%, a decline rate of 30.4% in total and 1.1% annually (Figure 5D).
Prevalence of age-related cancer incidence in China from 1990 to 2017. (A) population with cancer by age in China in 1990; (B) population with cancer by age in China in 2017; (C) prevalence of cancer by age in China from 1990 to 2017; (D) percentages of cancer prevalence by age in China from 1990 to 2019.
Cancer death attributed to non-genetic risk factors in 2019.
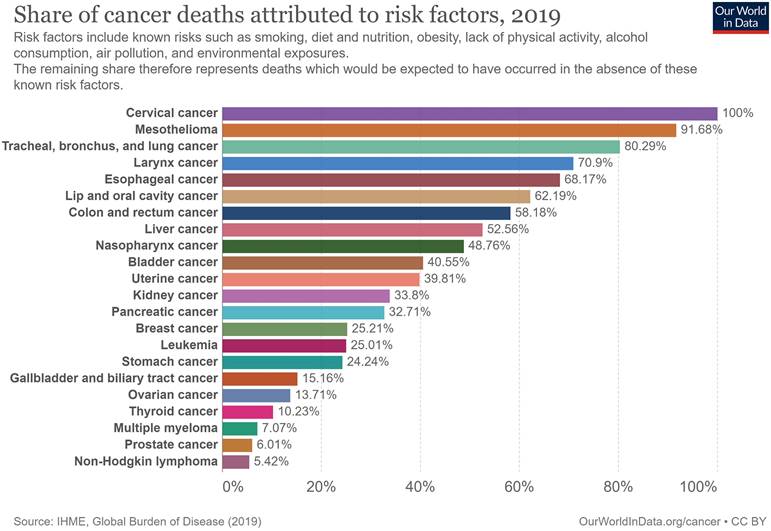
Cancer death related to economic and non-genetic risk factors
We found that the contribution of economic and non-genetic risk factors to cancer mortality differed, and many cancers appeared preventable and controllable. The non-genetic risk factors contributing to cervical cancer mortality risk were set as 100% (baseline); mortality risks of other cancers were lower than that of cervical cancer. The top five cancer-related deaths contributed by non-genetic risk factors were cervical cancer (100%), followed by mesothelioma (91.7%); tracheal, bronchial, and lung cancers (80.3%); laryngeal cancer (70.9%); esophageal cancer (68.2%); and lip and oral cavity cancer (62.2%). Among the other 6th to 22nd cancers, cancer deaths attributed to non-genetic risk factors were other digestive system cancers, urinary and reproductive system cancers, and hematological malignancies (Figure 6).
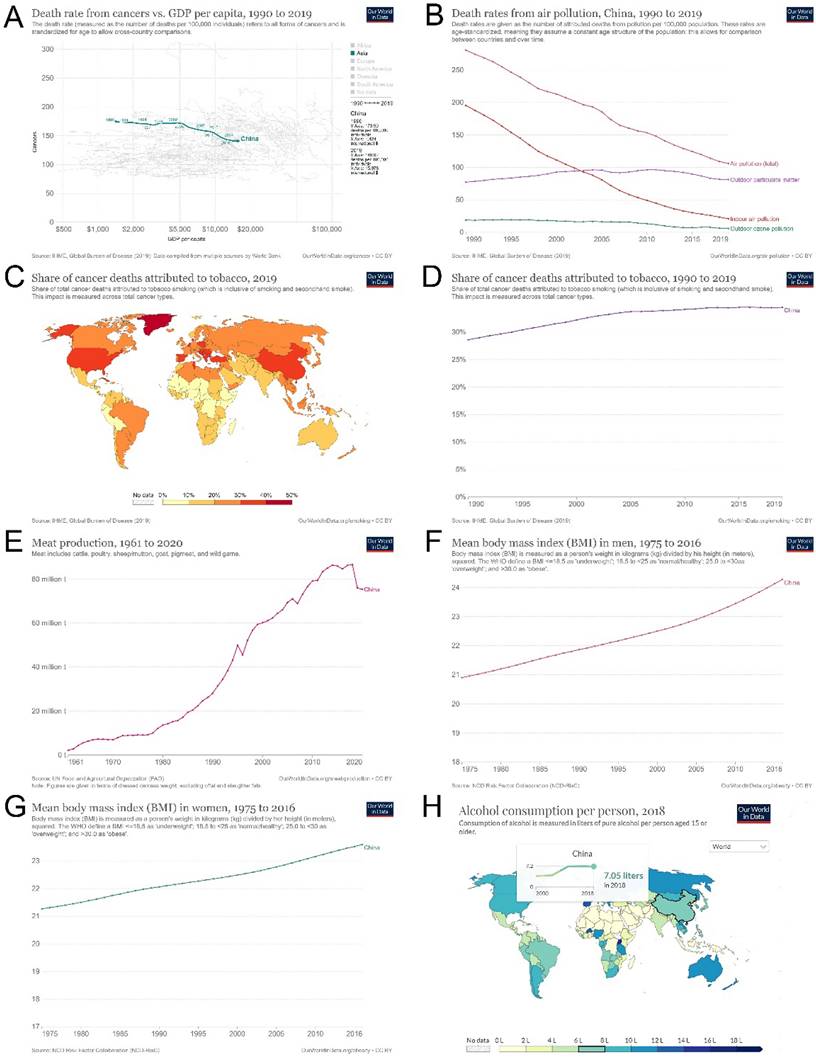
We found that China's economic development over the past 30 years has helped to reduce cancer mortality. With the annual increase in GDP, the cancer death rate decreased from 173.9/100,000 in 1990 to 140.9/100,000 in 2019. For every $1,000 increase in GDP, cancer deaths decreased by 2.3/100,000 (Figure 7A). Similarly, effectively controlling air pollution may reduce the mortality rate to a certain extent (Figure 7B). However, tobacco consumption in China remained high (28.62% in 1990 and 34.51% in 2019), was at a relatively high level worldwide, and tended to increase yearly, which is not conducive to cancer control (Figure 7C and D). In addition, the overall trend of unfavorable diet habits, such as meat consumption, increased evidently over the years (Figure 7E). The BMI of both men and women also increased annually (men, 21.9 kg/m2 in 1990 and 24.3 kg/m2 in 2016 (Figure 7F); women, 22.1 kg/m2 in 1990 and 23.6 kg/m2 in 2016 (Figure 7G). Furthermore, the overall trend of alcohol consumption increased over the past years, from 3.81 liters per person in 2000 to 7.05 liters per person in 2018 (Figure 7H). These unfavorable risk factors may contribute to the current increase in new-onset and cancer deaths.
Discussion
We found that tracheal, bronchial, and lung cancer surpassed gastric cancer as the leading cause of cancer mortality over the past 30 years, and its mortality rate increased at an annual rate of 6.5%. Tobacco exposure is a significant factor driving current trends in lung cancer [11]. Smoking rates have remained high in recent decades [2]. We found that the cancer mortality rate caused by smoking increased and has been at a high proportion worldwide. Additionally, a meta-analysis found that non-smokers with substantial exposure to secondhand smoke had a significantly increased overall cancer risk compared to those without such exposure (odds ratio (OR) of 1.163 (95% CI 1.058-1.279)); secondhand smoke significantly increased the risk of cancer in women (OR 1.253, 95% CI 1.142-1.374), including the risk of lung cancer (OR 1.245, 95% CI 1.026-1.511); thus, it was not only necessary to reduce active smoking but also to limit exposure to secondhand smoke [12]. China has set strict targets for tobacco control, and Healthy China 2030 targets to reduce smoking prevalence by 20% [7]. Therefore, smoking-related cancer morbidity and mortality may vary in the future. The overall trend of total lung cancer mortality in China is expected to decline over the next decade (2020-2030); however, the death rate is expected to continue to increase in the context of the aging population and high smoking rates in China [13]. The implementation of tobacco control programs faces multiple challenges. In addition to the enormous economic benefits of tobacco and other socioeconomic factors, it is difficult to impose a sudden ban on tobacco, considering individuals with tobacco abuse [14]. No significant difference in mean smoking cessation rates was observed between patients with/without cancer, regardless of whether smokers currently had cancer, were cancer survivors, or had a history of smoking-related cancers compared to those without a history of cancer [15].
The mortality and burden of digestive cancers vary widely. Cancer mortality rates of stomach, esophagus, and colorectal cancers increased slightly (annual growth rate, 1.3%-7.7%), whereas pancreatic cancer mortality rates increased rapidly (annual growth rate, 11.1%). Although the age-standardized burden of esophageal cancer has declined, new cases and deaths are predicted to continually increase [16]. Given the pattern of hepatitis B virus infection, China has long contributed to more than half of the global liver cancer burden in the past; however, a decline in the incidence of liver cancer across the country was observed recently, which may be related to the implementation of primary and secondary prevention interventions; it was predicted that liver cancer incidence in China may drop by 50% in 2050 [17]. The overall mortality trend of digestive system cancers (liver, stomach, and esophagus) in China is expected to decline over the next decade (2020-2030); however, the related deaths are expected to surge in the context of continued aging and high smoking rates [13]. Age-standardized rates of pancreatic cancer incidence and mortality increased from 1990 to 2019 and were higher in men than women; in particular, its incidence and mortality in the > 25 age group increased yearly [18]. The number of cases and deaths of pancreatic cancer is estimated to increase to 218,790 and 222,970 in 2030, respectively, an approximately 2-fold increase [19].
We found that the current proportion of reproductive system cancers was lower than that of lung and digestive system cancers; however, their incidence increased yearly; this may change the trend of cancer mortality and burden in the future. In men, the age-standardized incidence of prostate cancer in China increased by 12.6% from 2000 to 2011 (the highest rate of increase in cancers) [4]. In 2020, prostate cancer was the second most common malignant tumor in men worldwide, accounting for 14.1% of all male cancer incidence [20]. In women, the age-standardized incidence rates of breast, cervical, and ovarian cancers have also increased sharply in China [2]. Female breast cancer has surpassed lung cancer as the most commonly diagnosed cancer worldwide and ranks fifth in cancer deaths [20]. The impact of reproductive system cancer will increase sharply in the future [20,21]. Regarding risk factors, both smoking and secondhand smoke significantly increase the risk of breast cancer [12]. Tobacco control is expected to reduce the incidence and mortality of breast cancer to a certain extent.
Age is a critical factor in the incidence and mortality of cancer. Cancer mortality in all age groups in China has increased by 54.9% over the past 30 years. However, the age-standardized cancer mortality rate has decreased by 19.0% and 0.6% annually. Aging has increased cancer morbidity and mortality, and although aging did not increase the number of age-standardized cancer deaths, the percentage of cancer mortality across all age groups showed a noticeable increase. For example, the number of cancer deaths in the elderly aged ≥ 70 did not increase significantly; however, its percentage increased by 52.1% and 1.7% annually. By the end of 2022, there will be approximately 4.82 million and 2.37 million new cancer cases and 3.21 million and 640,000 cancer deaths in China and the United States, respectively; the increase in the number of the adult and aging population may be the main determinants of the increase in cancer deaths; therefore, active response to population aging may help reduce the cancer burden in China [21].
Cancer death attributed to economic and non-genetic risk factors in China since 1990. (A) GDP per capita and cancer death rates in China from 1990 to 2019; (B) air pollution and deaths in China from 1990 to 2019; (C) cancer deaths attributed to tobacco in the whole world in 2019; (D) cancer deaths attributed to tobacco in China from 1990 to 2019; (E) meat consumption in China from 1961 to 2020; (F) Mean body mass index in men in China from 1975 to 2016; (G) Mean body mass index in women in China from 1975 to 2016; (H) Alcohol consumption per person in China from 2000 to 2018.
Communicating diseases are not conducive to cancer control. The global pandemic, caused by a novel coronavirus called “severe acute respiratory syndrome coronavirus 2,” continues. Although the cause of death from COVID-19 is multiple organ dysfunction syndrome, patients with cancer are more susceptible to infection than those without cancer and seem to have a poorer prognosis due to their systemic immunosuppression status [22]. Chemotherapy within four weeks before the onset of COVID-19 symptoms is a risk factor for death during hospitalization [23]. A systematic review and meta-analysis found that patients with cancer were more susceptible to COVID-19 infection, and cancer increased the mortality rate of patients with COVID-19, among which patients with lung cancer had higher mortality rates than those without lung cancer [24]. Although vaccination against COVID-19 has helped to reduce its severe morbidity and mortality, there was considerable controversy regarding the vaccination for patients with cancer, including vaccine efficacy, the degree of humoral and cellular immune responses in these patients, and the incidence of vaccine-related adverse events [25]. This controversy has increased the difficulty of cancer epidemic prevention and control.
GDP has been associated with fewer cancer deaths. We found that for every $1,000 increase in China's GDP, cancer deaths decreased by 2.3/100,000. Although countries with higher GDP per capita have higher cancer incidence rates, the mortality rates have fallen substantially [26]. In countries with declining tobacco use, bladder cancer mortality was inversely related to per capita GDP [27]. GDP was also positively associated with testicular cancer incidence but negatively associated with testicular cancer mortality [28]. In addition, total health expenditure/GDP was related to a decrease in the ratio of morbidity and mortality of cancers such as stomach and lung cancers, suggesting that the total health expenditure was directly proportional to GDP and inversely proportional to the cancer mortality rate [29,30]. The increase in GDP has also contributed to the implementation of cancer research in China. Cancer research publications in China have proliferated over the past decade and surpassed the United States in 2018. Compared with other Asian countries, China's output was roughly proportional to its wealth [31], which may also contribute to a reduction in the mortality rate of patients with cancer. In addition, China's commitment to environmental pollution, such as effectively controlling air pollution, may also reduce the risk of cancer-related deaths [32].
Poor lifestyle habits increase the difficulty of cancer control. We found that China's meat and alcohol consumption showed an overall increasing trend, resulting in increased BMI every year. The study found that red meat consumption was associated with an increased risk of mortality from multiple hematological and solid cancers; an increase of 100 g of red meat per day was associated with an 11%-51% increase in the risk of multiple cancers, while an increase of 50 g per day of processed meat consumption was associated with an 8%-72% increase in cancers [33]. From 1990 to 2019, an increase in colorectal cancer mortality due to a high intake of processed meat was observed for both sexes in China; thus, gradually reducing the intake of processed meat may be an effective way to reduce colorectal cancer mortality [34]. We found that the current cancer risk corresponding to Chinese men's and women's BMI was within the controllable range. A study found that people with a BMI of approximately 22-25 had the lowest risk of cancer in the overall sample; however, a 1-unit increase in BMI was associated with a 5% increased risk of death in overweight participants (BMI 25.0-29.9) and 9% in obese participants (BMI ≥ 30.0). In comparison, a 34% and 14% lower risk was found in underweight (BMI < 18.5) and low-normal-weight participants, respectively [35]. With the development of the social economy, the BMI burden on cancer prevention and treatment will gradually increase if it is not controlled. The prevalence and number of individuals overweight and obese and associated medical costs are predicted to burden China's healthcare system by 2030. China has undertaken considerable to address obesity, including implementing related national policies and planning; however, these measures appear insufficient to control the obesity epidemic [36]. Globally, an estimated 741,300 or 4.1% of all new cancer cases in 2020 could be attributed to alcohol consumption, particularly alcohol-induced cancers such as the esophagus, liver, and breast; thus, measures are needed to increase awareness of alcohol use-related cancer risks and reduce overall alcohol consumption to prevent alcohol-induced cancer burden [37].
In China, both opportunities and challenges exist for cancer prevention and control. The continuous growth of China's GDP, effective control of environmental pollution, and popularization of clean energy will help reduce the incidence and mortality of cancer. In addition, China's progress and capabilities in cancer drug research and development and cancer clinical research have contributed to the management of patients with cancer. Furthermore, several recent health policies proposed by China have pointed to China's nutrition policy improvement over the next decade [38]. However, the number of cancer clinical trials with unique epidemiological characteristics in the Chinese population is small, and the geographical distribution is uneven. Therefore, it is necessary to address uniquely related and rare cancers in the Chinese population and the fairness, efficiency, and sustainability of cancer drug development [39]. Notably, the low participation rate in China's cancer screening, unevenly distributed medical resources, insufficient funds, and insufficient screening quality have caused difficulty in cancer control. In addition to addressing these issues, it is necessary to increase personnel training, optimize the definition of high-risk groups, and integrate new technologies into cancer screening programs in the future [40]. Furthermore, strengthening the 1st and 2nd levels of cancer prevention, particularly for those living in rural areas and vulnerable groups, would contribute to the overall control of cancer in China [1]. However, the frequent occurrence of communicable diseases worldwide, including in China, is not conducive to cancer screening and control. For example, cancer screening programs have been interrupted due to the onset of COVID-19, which has caused a delay in the diagnosis and, as a result, increased the mortality rate owing to cancer deaths that would have been avoidable in a pre-COVID era. Thus, urgent policy intervention is needed to address the backlog of routine diagnostic services and minimize the detrimental impact of the COVID-19 pandemic on patients with cancer [41].
This study had some limitations. Firstly, we did not re-analyze the data from "Our world in data"; thus, the results of this study were presented in descriptive form. Secondly, we gave the relative risk trends but did not analyze their correlations with cancer treads, morbidity, and mortality. Furthermore, this study did not include and analyze other cancer risks, such as the increasing population, the positive impact of medical technology advancements (cancer drug innovations, advances in surgical technology, etc.), and the effect of medical insurance policy on cancer incidence and death. In addition, China has a vast territory, and different regional food cultures differ significantly. Therefore, we did not give information about cancers with high incidence in different regions and their detailed change trend of cancer in different areas of China.
Conclusions
We summarized the developmental trends of morbidity and mortality of major cancers in China over the past 30 years and calculated their annual growth rates. Lung cancer has the highest morbidity and mortality rate. In addition, the mortality rates of pancreatic and colorectal cancer among digestive system cancers and prostate and breast cancers in the reproductive system show a rapidly increasing trend and need strengthening. We also analyzed the effects of GDP and changes in cancer risk factors on cancer incidence and mortality. Overall GDP growth and effective control of air pollution reduced cancer mortality, which, however, continued to increase owing to population aging, smoking, alcohol consumption, BMI, and meat consumption; these factors are adversely affecting cancer control. Hence, it is necessary to alert and educate society regarding the need for control.
Supplementary Material
Supplementary figure.
Acknowledgements
We were very grateful to the “Our world in data” team for giving us access to all their data and images and for their disdainful efforts to solve the world's major problems.
Funding
This study was supported by the Startup Fund for scientific research, Fujian Medical University (2019QH1050, WW), the Natural Science Foundation of Fujian Province (2022J05211, RZ), and China Urological Oncology Research Fund (#027) (YW).
Author Contributions
Conceptualization: WW, LL, and YW.
Formal analysis and investigation: WW, RZ, YJ, YL, SH, ZL, and TL.
Writing - original draft preparation: WW and YW.
Writing - review, and editing: YW and LL.
All authors read and approved the final manuscript.
Data Availability Statement
All data used in this study was available on the "Our world in data" (https://ourworldindata.org/).
Competing Interests
The authors have declared that no competing interest exists.
References
1. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F. et al. Cancer statistics in China, 2015. Ca Cancer J Clin. 2016;66:115-132
2. Sun D, Li H, Cao M, He S, Lei L, Peng J. et al. Cancer burden in china: trends, risk factors and prevention. Cancer Biol Med. 2020;17:879-895
3. Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in china: a secondary analysis of the global cancer statistics 2020. Chin Med J (Engl). 2021;134:783-791
4. Liu X, Zhou M, Wang F, Mubarik S, Wang Y, Meng R. et al. Secular trend of cancer death and incidence in 29 cancer groups in china, 1990-2017: a joinpoint and age-period-cohort analysis. Cancer Manag Res. 2020;12:6221-6238
5. Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in china: a time-trend analysis and comparison with the united states and united kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond). 2021;41:1037-1048
6. Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R. et al. Cancer registration in china and its role in cancer prevention and control. Lancet Oncol. 2020;21:e342-e349
7. The State Council of the People's Republic of China. China issues national nutrition plan (2017-2030) 2017 [cited 2022 Oct. 20]. Available from: http://english. www.gov.cn/policies/latest_releases/2017/07/13/content_281475725038850.htm
8. Goodchild M, Zheng R. Tobacco control and healthy china 2030. Tob Control. 2019;28:409-413
9. Roser M, Ritchie H. Cancer. Published online at ourworldindata. Org. Url: Https://Ourworldindata.Org/Cancer. 2015
10. Mathieu E, Ritchie H, Ortiz-Ospina E, Roser M, Hasell J, Appel C. et al. A global database of covid-19 vaccinations. Nat Hum Behav. 2021;5:947-953
11. Parascandola M, Xiao L. Tobacco and the lung cancer epidemic in china. Transl Lung Cancer Res. 2019;8:S21-S30
12. Kim AS, Ko HJ, Kwon JH, Lee JM. Exposure to secondhand smoke and risk of cancer in never smokers: a meta-analysis of epidemiologic studies. Int J Environ Res Public Health. 2018;15(9):1981
13. Li N, Wu P, Shen Y, Yang C, Zhang L, Chen Y. et al. Predictions of mortality related to four major cancers in china, 2020 to 2030. Cancer Commun (Lond). 2021;41:404-413
14. Jackson SE, Kotz D, West R, Brown J. Moderators of real-world effectiveness of smoking cessation aids: a population study. Addiction. 2019;114:1627-1638
15. Cinciripini PM, Karam-Hage M, Kypriotakis G, Robinson JD, Rabius V, Beneventi D. et al. Association of a comprehensive smoking cessation program with smoking abstinence among patients with cancer. Jama Netw Open. 2019;2:e1912251
16. Li S, Chen H, Man J, Zhang T, Yin X, He Q. et al. Changing trends in the disease burden of esophageal cancer in china from 1990 to 2017 and its predicted level in 25 years. Cancer Med. 2021;10:1889-1899
17. Shi JF, Cao M, Wang Y, Bai FZ, Lei L, Peng J. et al. Is it possible to halve the incidence of liver cancer in china by 2050? Int J Cancer. 2021;148:1051-1065
18. Zhu B, Wu X, Guo T, Guan N, Liu Y. Epidemiological characteristics of pancreatic cancer in china from 1990 to 2019. Cancer Control. 2021;28:1399497712
19. Chen J, Chen H, Zhang T, Yin X, Man J, Yang X. et al. Burden of pancreatic cancer along with attributable risk factors in china from 1990 to 2019, and projections until 2030. Pancreatology. 2022;22:608-618
20. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A. et al. Global cancer statistics 2020: globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca Cancer J Clin. 2021;71:209-249
21. Xia C, Dong X, Li H, Cao M, Sun D, He S. et al. Cancer statistics in china and united states, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135:584-590
22. Liang W, Guan W, Chen R, Wang W, Li J, Xu K. et al. Cancer patients in SARS-cov-2 infection: a nationwide analysis in china. Lancet Oncol. 2020;21:335-337
23. Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K. et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and covid-19 in hubei, china: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21:904-913
24. Yang L, Chai P, Yu J, Fan X. Effects of cancer on patients with covid-19: a systematic review and meta-analysis of 63,019 participants. Cancer Biol Med. 2021;18:298-307
25. Fendler A, de Vries E, GeurtsvanKessel CH, Haanen JB, Wormann B, Turajlic S. et al. Covid-19 vaccines in patients with cancer: immunogenicity, efficacy and safety. Nat Rev Clin Oncol. 2022;19:385-401
26. Wong MC, Goggins WB, Wang HH, Fung FD, Leung C, Wong SY. et al. Global incidence and mortality for prostate cancer: analysis of temporal patterns and trends in 36 countries. Eur Urol. 2016;70:862-874
27. Teoh JY, Huang J, Ko WY, Lok V, Choi P, Ng CF. et al. Global trends of bladder cancer incidence and mortality, and their associations with tobacco use and gross domestic product per capita. Eur Urol. 2020;78:893-906
28. Huang J, Chan SC, Tin MS, Liu X, Lok VT, Ngai CH. et al. Worldwide distribution, risk factors, and temporal trends of testicular cancer incidence and mortality: a global analysis. Eur Urol Oncol. 2022;5:566-576
29. Tsai MC, Wang CC, Lee HL, Peng CM, Yang TW, Chen HY. et al. Health disparities are associated with gastric cancer mortality-to-incidence ratios in 57 countries. World J Gastroenterol. 2017;23:7881-7887
30. Sung WW, Au KK, Wu HR, Yu CY, Wang YC. Improved trends of lung cancer mortality-to-incidence ratios in countries with high healthcare expenditure. Thorac Cancer. 2021;12:1656-1661
31. Li A, Lewison G. Chinese cancer research in 2009-18 and the disease burden. Cancer Manag Res. 2020;12:5031-5040
32. Chung CY, Yang J, Yang X, He J. Long-term effects of ambient air pollution on lung cancer and copd mortalities in china: a systematic review and meta-analysis of cohort studies. Environmental Impact Assessment Review. 2022;97:106865
33. Huang Y, Cao D, Chen Z, Chen B, Li J, Guo J. et al. Red and processed meat consumption and cancer outcomes: umbrella review. Food Chem. 2021;356:129697
34. Chen F, Chen S, Luo Y, Si A, Yang Y, Li Y. et al. Long-time trend of colorectal cancer mortality attributable to high processed meat intake in china and a bayesian projection from 2020 to 2030: a model-based study. Int J Environ Res Public Health. 2022;19(17):10603
35. Sun YQ, Burgess S, Staley JR, Wood AM, Bell S, Kaptoge SK. et al. Body mass index and all cause mortality in hunt and uk biobank studies: linear and non-linear mendelian randomisation analyses. Bmj. 2019;364:l1042
36. Wang Y, Zhao L, Gao L, Pan A, Xue H. Health policy and public health implications of obesity in china. Lancet Diabetes Endocrinol. 2021;9:446-461
37. Rumgay H, Shield K, Charvat H, Ferrari P, Sornpaisarn B, Obot I. et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol. 2021;22:1071-1080
38. Gao C, Xu J, Liu Y, Yang Y. Nutrition policy and healthy china 2030 building. Eur J Clin Nutr. 2021;75:238-246
39. Liang W, Guan W, Chen R, Wang W, Li J, Xu K. et al. Cancer patients in SARS-cov-2 infection: a nationwide analysis in china. Lancet Oncol. 2020;21:335-337
40. Cao M, Li H, Sun D, He S, Yu Y, Li J. et al. Cancer screening in china: the current status, challenges, and suggestions. Cancer Lett. 2021;506:120-127
41. Alkatout I, Biebl M, Momenimovahed Z, Giovannucci E, Hadavandsiri F, Salehiniya H. et al. Has covid-19 affected cancer screening programs? A systematic review. Front Oncol. 2021;11:675038
Author contact
![]() Corresponding authors: Yongbao Wei, Ph.D., weiybedu.cn; or Lin Le, M.D.linleedu.cn.
Corresponding authors: Yongbao Wei, Ph.D., weiybedu.cn; or Lin Le, M.D.linleedu.cn.

 Global reach, higher impact
Global reach, higher impact