3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(16):3139-3150. doi:10.7150/jca.87315 This issue Cite
Review
Digestive tract reconstruction after laparoscopic proximal gastrectomy for Gastric cancer: A systematic review
1. General Surgery, Cancer Center, Department of Gastrointestinal and Pancreatic Surgery, Zhejiang Provincial People's Hospital (Affiliated People's Hospital), Hangzhou Medical College, Hangzhou, Zhejiang, China. Key Laboratory of Gastroenterology of Zhejiang Province, Hangzhou, Zhejiang, China.
2. Zhejiang Chinese Medical University, Hangzhou, Zhejiang, China.
# These authors contributed equally to this work.
Abstract
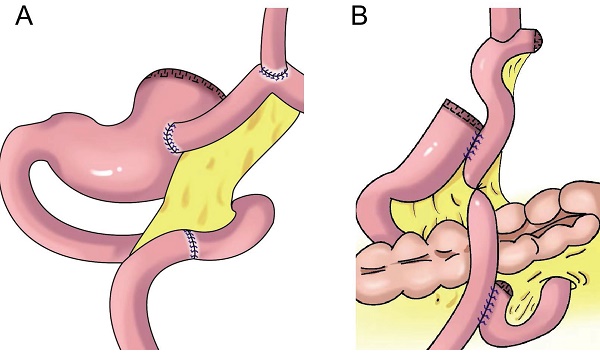
The incidence of gastroesophageal junction adenocarcinoma has gradually increased. Proximal gastrectomy or total gastrectomy is recommended for early gastric cancer of the upper third of the stomach. Because total gastrectomy is often accompanied by body mass loss and nutrient absorption disorders, such as severe hypoproteinemia and anemia, Proximal gastrectomy is more frequently recommended by researchers for early upper gastric cancer (T1N0M0) and Siewert II gastroesophageal junction cancer less than 4 cm in length. Although some functions of the stomach are retained after proximal gastrectomy, the anatomical structure of the gastroesophageal junction can be destroyed, and the anti-reflux effect of the cardia is lost. In recent years, as various reconstruction methods for anti-reflux function have been developed, some functions of the stomach are retained, and serious reflux esophagitis is avoided after proximal gastrectomy. In this article, we summarized the indications, advantages, and disadvantages of various classic reconstruction methods and latest improved reconstruction method including esophageal and residual stomach anastomosis, tubular gastroesophageal anastomosis, muscle flap anastomosis, jejunal interposition, and double-tract reconstruction.
Keywords: gastroesophageal junction adenocarcinoma, proximal gastrectomy, adenocarcinoma, tubular gastroesophageal anastomosis, muscle flap anastomosis, jejunal interposition, double-tract reconstruction

 Global reach, higher impact
Global reach, higher impact