Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(2):473-483. doi:10.7150/jca.87881 This issue Cite
Research Paper
Impact of Treatment Delay on the Prognosis of Patients with Ovarian Cancer: A Population-based Study Using the Surveillance, Epidemiology, and End Results Database
Department of Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, China.
* Jing Zhao and Ruiying Chen contributed equally to this work.
Received 2023-7-7; Accepted 2023-10-22; Published 2024-1-1
Abstract
Purpose: This study aimed to assess the impact of treatment delay on prognosis in patients with ovarian cancer.
Methods: A retrospective analysis of patients with ovarian cancer in the Surveillance, Epidemiology, and End Results (SEER) database between 2010 and 2015 was performed. Chi-square tests were used to assess baseline differences. The Kaplan-Meier method was used to evaluate the effect of different treatment intervals on survival outcomes in patients. Cox regression analyses were used to identify independent factors associated with ovarian cancer prognosis.
Results: Of the 21,590 patients included, 15,675 (72.6%), 5,582 (25.9%), and 333 (1.54%) were classified into the immediate-treatment (<1 month after diagnosis), intermediate-delay (1-2 month delayed), and long-delay groups (≥3 months delayed), respectively. The 5-year probability of overall survival (OS) was 61.4% in the immediate-treatment group, decreasing to 36.4% and 34.8% in the intermediate- and long-delay groups, respectively. Similar survival differences were also reflected in cancer-specific survival (CSS), with 5-year CSS probabilities of 66.7%, 42.6%, and 41.8% in the aforementioned groups, respectively. Patients in the intermediate-delay group showed poorer OS (adjusted hazard ratio [HR], 1.06; 95% confidence interval [CI], 1.02-1.11; p=0.006) and CSS (adjusted HR, 1.06; 95% CI, 1.01-1.11; p=0.012) than immediate-treatment group.
Conclusions: Patients with delayed treatment had poorer OS and CSS. The patient's waiting time from diagnosis to initial treatment should be within 1 month.
Keywords: Ovarian cancer, Treatment delay intervals, SEER, Prognosis, Retrospective
Introduction
According to the latest statistics, there were approximately 12,810 deaths and 19,880 new diagnoses of ovarian cancer in the United States in 2022 [1]. Despite improvements in therapeutics, the 5-year overall survival (OS) rate remains below 50% [2]. Several studies have reported a number of clinical features that may influence the prognosis of ovarian cancer [3-6]. Delays in cancer treatment are common and were particularly common during the COVID-19 pandemic. Whether delaying treatment affects the clinical outcome of ovarian cancer is currently unclear. A study looking at different referral methods for patients with ovarian, lung, prostate, and colorectal cancer found that delayed referral had no effect on survival for ovarian cancer patients [7]. Pyeon et al. [8] reported that delaying palliative chemotherapy had no adverse effects on the survival of patients with recurrent ovarian cancer. Delayed chemotherapy had no effect on the chemotherapy efficacy and declined levels of cancer antigen (CA) 125 during the coronavirus disease 2019 (COVID-19) pandemic [9].
Clearly, few studies have reported the impact of delayed treatment on the prognosis of patients with ovarian cancer, and few criteria are currently available for assessing the time intervals associated with delayed treatment in patients with ovarian cancer. Using the national sample of patient data obtained from the Surveillance, Epidemiology, and End Results (SEER) database, this study analyzed the detailed information of patients with delayed treatment. The aim is to assess the detrimental effect of delayed treatment on patient outcomes, as well as the patient characteristics for which delayed treatment has a greater impact on prognosis, in order to provide new guidance for treatment.
Methods
Data and Variables
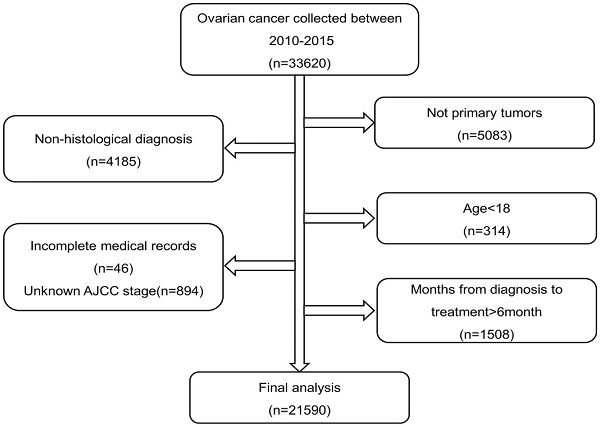
SEER*Stat version 8.4.0.1 (https://seer.cancer.gov/seerstat/) was used to obtain patient data from SEER 17 Registries Database during 2010 to 2015. The inclusion criteria were as follows: (1) patients with ovarian cancer initially screened using the International Classification of Oncological Diseases 3 (ICD-O-3) code whose diagnosis was confirmed pathologically and (2) patients with primary ovarian cancer as their first cancer. The exclusion criteria were as follows: (1) patients survival time was 0, (2) patients with incomplete histological and staging information, (3) patients aged <18 years, and (4) treatment delays of >6 months owing to statistically invalid results because of the small sample size. From the SEER database, we initially extracted 28,537 patients diagnosed with ovarian cancer. A total of 6,947 patients were excluded; hence, 21,590 patients were finally included. The detailed exclusion criteria is shown in Figure 1. The tumor stage of patients was extracted according to the American Joint Committee on Cancer (AJCC), 7th edition. The ICD-O-3 code was selected to identify histological types.
Flow chart of patient selection from the SEER database
Variables, including age, marital status, race, rural/urban, median household income, regional lymph node examination, distant metastasis, stage, histological type, grade of differentiation, therapy, residual tumor and surgery were included in the study. Race was classified as white, black, or other/unknown (e.g., Hispanic, Asian, and so on). The category 'other epithelial disorders' contains less specific and/or diagnostic combinations. The therapy was classified as 'neoadjuvant chemotherapy (NACT)', 'primary surgical therapy', or 'no chemotherapy and/or surgery'. The surgery was classified as 'local resection', 'debulking surgery', 'pelvic exenteration', or 'Unknown'. The residual tumor was classified as 'no residual lesion', '≤1 cm', '>1 cm', or 'Unknown'.
The data on treatment time intervals in this study were from the variable 'Months from diagnosis to treatment' in the SEER database. The database handbook states that treatment could include surgery, radiation therapy, chemotherapy, hormone, immunotherapy, and/or active surveillance. Currently, there are no guidelines or consensus defining a specific time interval for treatment delays. According to previous studies [10-12], an initial treatment of ≥1 month is considered delayed treatment, whereas an interval of ≥3 months is considered a long-delay treatment. We divided patients into three groups: immediate-treatment (<1 month), intermediate-delayed (1-2 months), and long-delay (≥3 months).
Statistical analysis
The Chi-square test and Kruskal-Wallis test were used to detect variables among the three groups. Univariate and multivariate Cox regression analyses were used to identify independent risk factors. Kaplan-Meier analyses were used to calculate survival rates. SPSS version 22.0 (IBM Corp., Armonk, NY, USA) and R version 4.2.2 (www.r-project.org) were used for statistical analyses. A two-tailed p-value <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
The baseline data of 21,590 patients are compared in Table 1. Of these patients, 15,675 (72.6%), 5582 (22.7%), and 333 (1.5%) received immediate-treatment (<1 month), intermediate-delay treatment (1-2 months) and long-delay treatment (≥3 months) following diagnosis. Age, marital status, race, regional lymph node examination, distant organ metastasis, stage, histology, grade, surgery, therapy and residual status significantly differed across the three groups. The median age of patients in the immediate-treatment, intermediate-delay treatment, and long-delay treatment groups was 58 (interquartile range [IQR], 49-67), 64 (IQR, 55-72), and 63 (IQR, 54-71) years (p<0.001), respectively. In the long-delay group, single patients comprised 57.7%, whereas married patients accounted for only 39.0% (p<0.001). The distribution of different races was different among the three groups (p <0.001). Differences were also observed during lymph node examination: 43.1% of patients in the immediate-treatment group had negative regional lymph node examination results (p <0.001). Moreover, we noted differences in the treatment times on distant metastases. In the immediate-treatment group, patients without distant metastasis comprised 83.6% of the cohort, whereas patients with distant metastasis accounted for only 15.6%. In the intermediate- and long-delayed groups, the number of patients without metastasis dropped to 58.2% and 54.4% (p <0.001), respectively. Most patients with advanced stages experienced delayed treatment. Among patients with intermediate-delay treatment, stage III and IV patients comprised 44.8% and 40.9% of the cohort, respectively; stage III and IV patients comprised 37.8% and 42.9% of those who underwent long-delay treatment (p <0.001), respectively. Histology was differentially distributed among the three cohorts (p <0.001). Approximately 50% of patients (range, 44.4-53.1%) had poorly differentiated/undifferentiated tumor status, and tissue differentiation was significantly different among the three groups (p <0.001). Of 38.1% patients in the immediate-treatment group received debulking surgery, while 50.1% of patients in the intermediate-delayed treatment group received debulking surgery (P <0.001). More than half (62.6%) of the patients in the immediate-treatment group received primary surgical therapy, and only 8.5% of the patients received NACT (P <0.001). There was a difference in residual tissue size between the three groups of patients (p < 0.001).
Overall, in the immediate-treatment group, the predominant ethnic group was White (67.3%), and the immediate-treatment group had the youngest patient (age, 58 [IQR, 49-67]), highest survival rate (56.1%), and lowest death rate from ovarian cancer (35.8%).
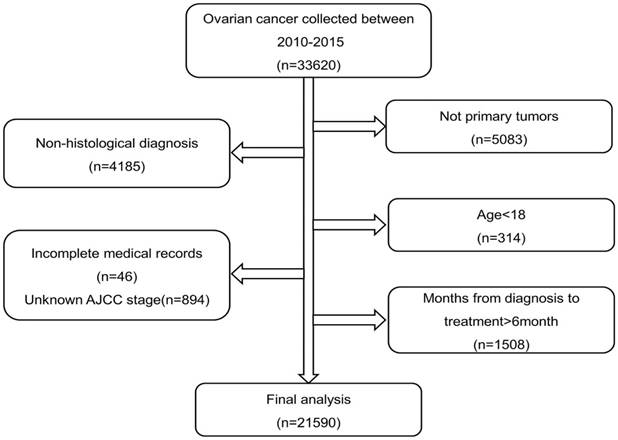
Effect of treatment delay on OS
The study population from the SEER database was followed up until November 2021. A total of 10,922 (50.6%) patients died, and the median survival time was 54 (IQR, 25-79) months. The 2-year survival rate of all patients was 87.0%, the 5-year survival rate was 54.5%, and the 10-year survival rate was 40.0%. The median survival times in the immediate, intermediate-delay, and long-delay treatment groups were 59, 40, and 39 months, respectively. The 5-year OS rates of patients in the aforementioned groups were 61.4%, 36.4%, and 34.8%, respectively (p <0.001) (Figure 2).
Baseline characteristics of patients with different time delay intervals 2010 to 2015(n=21590)
| Variables | Immediate n=15675 | Intermediate -delay n=5582 | Long-delay n=333 | P-value |
|---|---|---|---|---|
| Age | 58(IQR, 49-67) | 64(IQR, 55-72) | 63(IQR,54-71) | <0.001 |
| Marriage | <0.001 | |||
| Married | 8288(52.9) | 2756(49.4) | 130(39.0) | |
| Single | 6730(42.9) | 2582(46.3) | 192(57.7) | |
| Unknown | 657(4.2) | 244(4.4) | 11(3.3) | |
| Race | <0.001 | |||
| Black | 1059(6.8) | 473(8.5) | 53(15.9) | |
| White | 10554(67.3) | 3802(68.1) | 167(50.2) | |
| Other | 4062(25.9) | 1307(23.4) | 113(33.9) | |
| Rural-Urban | 0.091 | |||
| Metropolitan | 14091(89.9) | 4996(89.5) | 310(93.1) | |
| Nonmetropolitan | 1573(10.0) | 577(10.3) | 23(6.9) | |
| Unknown | 11(0.1) | 9(0.2) | 0(0.0) | |
| Median household income inflation | 0.091 | |||
| < $35,000 | 227(1.4) | 70(1.3) | 4(1.2) | |
| $35,000 - $55,000 | 3001(19.1) | 1069(19.2) | 68(20.4) | |
| $55,000 - $75,000 | 7623(48.6) | 2786(49.9) | 181(54.4) | |
| >$75,000 | 4824(30.8) | 1657(29.7) | 80(24.0) | |
| Regional nodes | <0.001 | |||
| Negative | 6761(43.1) | 1270(22.8) | 75(22.5) | |
| Positive | 2590(16.5) | 1054(18.9) | 58(17.4) | |
| Not detected | 6207(39.6) | 3190(57.1) | 196(58.9) | |
| Unknown | 117(0.7) | 68(1.2) | 4(1.2) | |
| Metastases at distance | <0.001 | |||
| Negative | 13103(83.6) | 3249(58.2) | 181(54.4) | |
| Positive | 2447(15.6) | 2284(40.9) | 143(42.9) | |
| Unknown | 125(0.8) | 49(0.9) | 9(2.7) | |
| Stage | <0.001 | |||
| I | 5600(35.7) | 486(8.7) | 42(12.6) | |
| II | 1797(11.5) | 314(5.6) | 22(6.6) | |
| III | 5831(37.2) | 2498(44.8) | 126(37.8) | |
| IV | 2447(15.6) | 2284(40.9) | 143(42.9) | |
| Histology | <0.001 | |||
| Serous | 9000(57.4) | 4365(78.2) | 229(68.8) | |
| Mucinous | 1134(7.2) | 160(2.9) | 18(5.4) | |
| Endometrioid | 1983(12.7) | 298(5.3) | 21(6.3) | |
| Clear | 1272(8.1) | 206(3.7) | 14(4.2) | |
| Other epithelial | 931(5.9) | 413(7.4) | 24(7.2) | |
| Non-epithelial | 1355(8.6) | 140(2.5) | 27(8.1) | |
| Grade | <0.001 | |||
| Well differentiated | 1589(10.1) | 206(3.7) | 17(5.1) | |
| Moderately differentiated | 2179(13.9) | 406(7.3) | 26(7.8) | |
| Poorly differentiated/undifferentiated | 8326(53.1) | 3233(57.9) | 148(44.4) | |
| Unknown | 3581(22.8) | 1737(31.1) | 142(42.6) | |
| Cause of death | <0.001 | |||
| Alive | 8787(56.1) | 1780(31.9) | 101(30.3) | |
| Ovarian cancer | 5611(35.8) | 3188(57.1) | 190(57.1) | |
| Other cause | 1277(8.1) | 614(11.0) | 42(12.6) | |
| Survival months | 59(IQR,30-83) | 40(IQR,18-63) | 39(IQR,18-60.5) | <0.001 |
| Surgery | <0.001 | |||
| Local resection | 8789(56.1) | 1695(30.4) | 126(37.8) | |
| Debulking surgery | 5967(38.1) | 2795(50.1) | 110(33.0) | |
| Pelvic exenteration | 243(1.6) | 99(1.8) | 6(1.8) | |
| Unknown | 676(4.3) | 993(17.8) | 91(27.3) | |
| Therapy | <0.001 | |||
| NACT | 1336(8.5) | 1671(29.9) | 84(25.2) | |
| Primary surgical therapy | 9809(62.6) | 2458(44.0) | 101(30.3) | |
| No chemotherapy and/or surgery | 4530(28.9) | 1453(26.0) | 148(44.4) | |
| Residual | <0.001 | |||
| No residual lesion | 7105(45.3) | 1649(29.5) | 83(24.9) | |
| ≤1cm | 1080(6.9) | 676(12.1) | 19(5.7) | |
| >1cm | 1407(9.0) | 750(13.4) | 48(14.4) | |
| Unknown | 6083(38.8) | 2507(44.9) | 183(55.0) |
Abbreviation NACT: Neoadjuvant chemotherapy
Kaplan-Meier curve of overall survival according to months from diagnosis to treatment
Subsequently, we explored the factors affecting OS in ovarian cancer using univariate and multivariate Cox regression. Months from diagnosis to treatment, age, race, marital status, household income, tissue differentiation, stage, histology, therapy and residual tumor were independent risk factors of OS in patients with ovarian cancer (Table 2). Of note, after adjusting for other confounders, the intermediate-delay group (1-2-month delay) showed a worse OS compared with the immediate-treatment group (adjusted hazard ratio [HR], 1.06; 95% confidence interval [CI], 1.02-1.11; p=0.005) (Table 2).
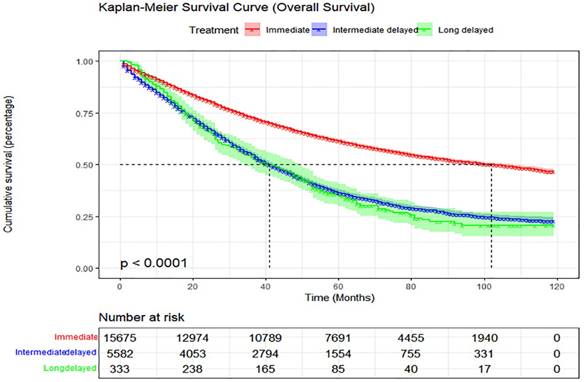
Effect of treatment delay on cancer-specific survival (CSS)
The 5-year CSS rates also differed significantly among the three groups, with rates of 66.7%, 42.6%, and 41.8%, respectively (Figure 3). We explored the factors affecting CSS in patients with ovarian cancer using univariate and multivariate Cox analyses. Months from diagnosis to treatment, age, race, marital status, household income, tissue differentiation, stage, histology, therapy and residual were identified as independent predictors of CSS (Table 3). After adjusting for interference factors, the intermediate-delay (1-2-month delay) group had significantly impaired CSS (adjusted HR, 1.06; 95% CI, 1.01-1.11; p=0.010) (Table 3).
Survival at different treatment delay intervals after subgroup stratification
We performed a stratified analysis based on histological type and stage (Table 4). Compared with the immediate-treatment group, among patients with serous tumor stage I/II, the long-delay group had a 2.65 times higher risk of mortality (OS: HR, 2.65; 95% CI, 1.40-5.01; p =0.003) and a 2.41 times higher risk of cancer-specific mortality (CSS: HR, 2.41; 95% CI, 1.13-5.17; p=0.023), and among patients with serous ovarian tumor stage III/ IV, both the mortality and cancer-specific mortality risk rate in the intermediate-delay group increased (OS: HR, 1.09; 95% CI, 1.04-1.15; p<0.001; CSS:HR, 1.09; 95% CI, 1.03-1.15; p=0.002) (Table 4). The same was true for patients with clear cell tumor stage I/II (Table 4).
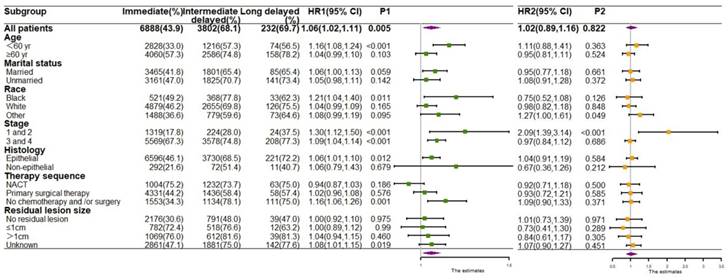
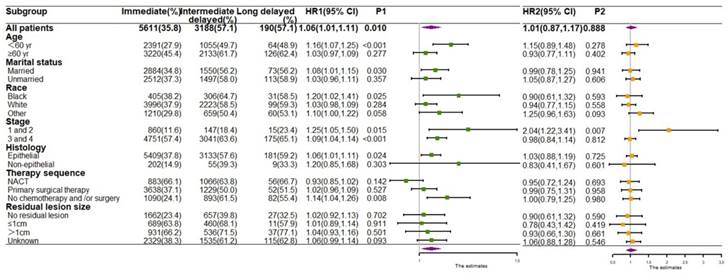
Moreover, to describe which characteristics of patients with delayed treatment lead to a worse prognosis, we performed stratified analyses based on both demographic and clinical characteristics to observe the OS (Figure 4) and CSS (Figure 5) of patients. For patients aged <60 years, who were black, were in stage I/II, had epithelial ovarian tumors, and had not undergo chemotherapy and/or surgery, both OS and CSS risks were significantly increased if they received intermediate- delay treatment. Additionally, the highest mortality and cancer-specific mortality risk values were observed in the long-delay group in patient with stage I/II (OS: HR, 2.09; 95% CI, 1.39-3.14; p <0.001; CSS:HR, 2.04; 95% CI, 1.22-3.41; p=0.007) (Figure 4 and Figure 5).
Discussion
Delays in cancer treatments are common, and treatment may be delayed for reasons such as insurance, seeking a second opinion, imaging evaluation, referral and prehabilitation. A retrospective study of 1,463 ovarian cancer patients by Nagle et al. [13] found that once symptoms of ovarian cancer appear, delay in diagnosis does not adversely affect survival. A systematic review covering various types of cancer comprehensively analyzed 209 trials in 177 articles and concluded that timely diagnosis and treatment of symptomatic cancer patients can improve the survival rate of patients [14]. Noer MC et al. [15] reported that the impact of ovarian cancer comorbidities on survival appears to be independent of systemic delays. More recently, Sud, A et al. [16] reported that a delay of 3/6 months in surgery for incident cancers would result in a 19%/43% reduction in life years gained. Overall, there is currently no consensus on the relationship between the timing of ovarian cancer patients' initial treatment and their prognosis. Importantly, due to reduced travel and controlled administration, delays in treatment were more pronounced during the COVID-19 pandemic [17]. Therefore, insight into the prognostic impact of treatment delays is essential.
Univariate and multivariate analyses of the association of treatment delay intervals with overall survival (OS)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Variables | HR (95% CI) | P-value | HR (95% CI) | P-value |
| Months from diagnosis to treatment | ||||
| Immediate | 1.00(ref) | ref | 1.00(ref) | ref |
| Intermediate-delay | 1.99(1.91,2.07) | <0.001 | 1.06(1.02,1.11) | 0.005 |
| Long-delay | 2.08(1.82,2.37) | <0.001 | 1.02(0.89,1.16) | 0.822 |
| Age | 1.04(1.04,1.04) | <0.001 | 1.02(1.02,1.02) | <0.001 |
| Race | ||||
| Black | 1.00(ref) | ref | 1.00(ref) | ref |
| White | 0.81(0.76,0.87) | <0.001 | 0.82(0.77,0.88) | <0.001 |
| Other | 0.65(0.60,0.70) | <0.001 | 0.81(0.75,0.88) | <0.001 |
| Rural-Urban | ||||
| Metropolitan | 1.00(ref) | ref | 1.00(ref) | ref |
| Nonmetropolitan | 1.14(1.07,1.21) | <0.001 | 1.01(0.95,1.09) | 0.688 |
| Unknown | 1.52(0.90,2.57) | 0.114 | 1.28(0.76,2.17) | 0.360 |
| Marriage | ||||
| Married | 1.00(ref) | ref | 1.00(ref) | ref |
| Single | 1.22(1.17,1.26) | <0.001 | 1.16(1.11,1.20) | <0.001 |
| Unknown | 1.06(0.96,1.17) | 0.227 | 0.98(0.89,1.08) | 0.750 |
| Median household income inflation | ||||
| < $35,000 | 1.00(ref) | ref | 1.00(ref) | ref |
| $35,000 - $55,000 | 0.90(0.77,1.05) | 0.177 | 0.96(0.82,1.13) | 0.623 |
| $55,000 - $75,000 | 0.78(0.67,0.91) | 0.001 | 0.86(0.73,1.02) | 0.079 |
| >$75,000 | 0.73(0.62,0.85) | <0.001 | 0.83(0.70,0.98) | 0.026 |
| Stage | ||||
| I | 1.00(ref) | ref | 1.00(ref) | ref |
| II | 2.80(2.54,3.10) | <0.001 | 2.80(2.53,3.11) | <0.001 |
| III | 6.91(6.43,7.43) | <0.001 | 5.93(5.45,6.45) | <0.001 |
| IV | 11.34(10.52,12.22) | <0.001 | 8.23(7.53,8.99) | <0.001 |
| Histology | ||||
| Serous | 1.00(ref) | ref | 1.00(ref) | ref |
| Mucinous | 0.34(0.31,0.38) | <0.001 | 1.49(1.32,1.68) | <0.001 |
| Endometrioid | 0.27(0.25,0.30) | <0.001 | 0.84(0.76,0.92) | <0.001 |
| Clear | 0.49(0.45,0.54) | <0.001 | 1.39(1.27,1.52) | <0.001 |
| Other epithelial | 1.42(1.33,1.52) | <0.001 | 1.44(1.35,1.55) | <0.001 |
| Non-epithelial | 0.32(0.29,0.36) | <0.001 | 0.95(0.85,1.06) | 0.363 |
| Grade | ||||
| Well differentiated | 1.00(ref) | ref | 1.00(ref) | ref |
| Moderately differentiated | 2.23(1.95,2.55) | <0.001 | 1.66(1.44,1.90) | <0.001 |
| Poorly differentiated/undifferentiated | 5.16(4.58,5.82) | <0.001 | 1.98(1.74,2.25) | <0.001 |
| Unknown | 4.90(4.33,5.54) | <0.001 | 1.88(1.65,2.14) | <0.001 |
| Therapy | ||||
| NACT | 1.00(ref) | ref | 1.00(ref) | ref |
| Primary surgical therapy | 0.50(0.47,0.52) | <0.001 | 0.91(0.86,0.96) | <0.001 |
| No chemotherapy and/or surgery | 0.54(0.51,0.57) | <0.001 | 1.50(1.41,1.59) | <0.001 |
| Residual | ||||
| No residual lesion | 1.00(ref) | ref | 1.00(ref) | ref |
| ≤1cm | 3.00(2.81,3.20) | <0.001 | 1.57(1.47,1.68) | <0.001 |
| >1cm | 3.48(3.28,3.70) | <0.001 | 1.74(1.63,1.85) | <0.001 |
| Unknown | 2.11(2.02,2.21) | <0.001 | 1.45(1.38,1.52) | <0.001 |
Abbreviation NACT: Neoadjuvant chemotherapy
Kaplan-Meier curve of cancer-specific survival according to months from diagnosis to treatment
Univariate and multivariate analyses of the association of treatment delay intervals with cancer-specific survival (CSS)
| Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|
| Variables | HR (95% CI) | P-value | HR (95% CI) | P-value |
| Months from diagnosis to treatment | ||||
| Immediate | 1.00(ref) | ref | 1.00(ref) | ref |
| Intermediate-delay | 2.03(1.95,2.12) | <0.001 | 1.06(1.01,1.11) | 0.010 |
| Long-delay | 2.07(1.79,2.40) | <0.001 | 1.01(0.87,1.17) | 0.888 |
| Age | 1.03(1.03,1.04) | <0.001 | 1.02(1.01,1.02) | <0.001 |
| Race | ||||
| Black | 1.00(ref) | ref | 1.00(ref) | ref |
| White | 0.83(0.77,0.90) | <0.001 | 0.84(0.78,0.91) | <0.001 |
| Other | 0.66(0.61,0.72) | <0.001 | 0.82(0.76,0.90) | <0.001 |
| Rural-Urban | ||||
| Metropolitan | 1.00(ref) | ref | 1.00(ref) | ref |
| Nonmetropolitan | 1.12(1.05,1.20) | 0.001 | 1.02(0.94,1.10) | 0.679 |
| Unknown | 1.31(0.71,2.44) | 0.389 | 1.09(0.59,2.04) | 0.779 |
| Marriage | ||||
| Married | 1.00(ref) | ref | 1.00(ref) | ref |
| Single | 1.16(1.11,1.21) | <0.001 | 1.13(1.08,1.18) | <0.001 |
| Unknown | 1.02(0.92,1.14) | 0.702 | 0.96(0.86,1.07) | 0.485 |
| Median household income inflation | ||||
| < $35,000 | 1.00(ref) | ref | 1.00(ref) | ref |
| $35,000 - $55,000 | 0.90(0.76,1.06) | 0.212 | 0.95(0.79,1.13) | 0.541 |
| $55,000 - $75,000 | 0.80(0.68,0.95) | 0.010 | 0.88(0.73,1.05) | 0.160 |
| >$75,000 | 0.74(0.62,0.87) | <0.001 | 0.83(0.69,0.99) | 0.042 |
| Stage | ||||
| I | 1.00(ref) | ref | 1.00(ref) | ref |
| II | 3.52(3.11,3.98) | <0.001 | 3.39(2.99,3.85) | <0.001 |
| III | 10.12(9.22,11.10) | <0.001 | 8.01(7.21,8.89) | <0.001 |
| IV | 16.14(14.68,17.75) | <0.001 | 10.86(9.74,12.11) | <0.001 |
| Histology | ||||
| Serous | 1.00(ref) | ref | 1.00(ref) | ref |
| Mucinous | 0.26(0.22,0.29) | <0.001 | 1.33(1.15,1.54) | <0.001 |
| Endometrioid | 0.20(0.18,0.22) | <0.001 | 0.69(0.61,0.78) | <0.001 |
| Clear | 0.49(0.44,0.53) | <0.001 | 1.49(1.34,1.64) | <0.001 |
| Other epithelial | 1.37(1.27,1.48) | <0.001 | 1.43(1.33,1.55) | <0.001 |
| Non-epithelial | 0.27(0.24,0.31) | <0.001 | 0.86(0.75,0.98) | 0.022 |
| Grade | ||||
| Well differentiated | 1.00(ref) | ref | 1.00(ref) | ref |
| Moderately differentiated | 2.95(2.48,3.51) | <0.001 | 1.99(1.67,2.38) | <0.001 |
| Poorly differentiated/undifferentiated | 7.64(6.53,8.95) | <0.001 | 2.44(2.07,2.88) | <0.001 |
| Unknown | 6.86(5.85,8.06) | <0.001 | 2.29(1.94,2.71) | <0.001 |
| Therapy | ||||
| NACT | 1.00(ref) | ref | 1.00(ref) | ref |
| Primary surgical therapy | 0.49(0.46,0.51) | <0.001 | 0.89(0.84,0.94) | <0.001 |
| No chemotherapy and/or surgery | 0.46(0.43,0.49) | <0.001 | 1.39(1.30,1.49) | <0.001 |
| Residual | ||||
| No residual lesion | 1.00(ref) | ref | 1.00(ref) | ref |
| ≤1cm | 3.37(3.14,3.61) | <0.001 | 1.65(1.54,1.77) | <0.001 |
| >1cm | 3.87(3.63,4.13) | <0.001 | 1.83(1.71,1.96) | <0.001 |
| Unknown | 2.20(2.09,2.31) | <0.001 | 1.50(1.42,1.58) | <0.001 |
Abbreviation NACT: Neoadjuvant chemotherapy
Multivariate analyses of the association of treatment delay intervals with OS and CSS
| Tumor | Subgroupc | OS | CSS | |||
|---|---|---|---|---|---|---|
| HRa (95% CI) | P-value | HRb(95% CI) | P-value | |||
| Serous | Stage I/II | Intermediate-delay | 1.20(0.97,1.47) | 0.094 | 1.09(0.85,1.40) | 0.508 |
| Long-delay | 2.65(1.40,5.01) | 0.003 | 2.41(1.13,5.17) | 0.023 | ||
| Stage III/IV | Intermediate-delay | 1.09(1.04,1.15) | <0.001 | 1.09(1.03,1.15) | 0.002 | |
| Long-delay | 1.07(0.91,1.25) | 0.396 | 1.09(0.92,1.29) | 0.332 | ||
| Mucinous | Stage I/II | Intermediate-delay | 1.28(0.75,2.18) | 0.367 | 1.68(0.84,3.35) | 0.144 |
| Long-delay | 2.44(0.86,6.91) | 0.092 | 2.04(0.47,8.87) | 0.344 | ||
| Stage III/IV | Intermediate-delay | 1.01(0.71,1.44) | 0.941 | 0.85(0.55,1.29) | 0.444 | |
| Long-delay | 0.37(0.13,1.09) | 0.073 | 0.48(0.14,1.66) | 0.246 | ||
| Endometrioid | Stage I/II | Intermediate-delay | 1.11(0.74,1.65) | 0.618 | 1.41(0.84,2.37) | 0.192 |
| Long-delay | 2.10(0.76,5.77) | 0.151 | 1.63(0.22,11.91) | 0.632 | ||
| Stage III/IV | Intermediate-delay | 1.07(0.80,1.42) | 0.664 | 0.94(0.67,1.32) | 0.720 | |
| Long-delay | 1.31(0.55,3.13) | 0.536 | 0.80(0.24,2.67) | 0.716 | ||
| Clear | Stage I/II | Intermediate-delay | 1.87(1.28,2.73) | 0.001 | 1.91(1.23,2.96) | 0.004 |
| Long-delay | 2.44(0.74,8.05) | 0.144 | 2.69(0.63,11.42) | 0.180 | ||
| Stage III/IV | Intermediate-delay | 1.11(0.84,1.45) | 0.461 | 1.28(0.97,1.70) | 0.081 | |
| Long-delay | 0.49(0.21,1.15) | 0.102 | 0.60(0.25,1.40) | 0.236 | ||
| Other epithelial | Stage I/II | Intermediate-delay | 1.40(0.83,2.35) | 0.208 | 0.80(0.38,1.69) | 0.558 |
| Long-delay | 1.18(0.16,8.82) | 0.872 | 2.01(0.26,15.59) | 0.502 | ||
| Stage III/IV | Intermediate-delay | 1.04(0.89,1.21) | 0.648 | 1.06(0.90,1.26) | 0.488 | |
| Long-delay | 0.77(0.47,1.25) | 0.290 | 0.72(0.41,1.27) | 0.261 | ||
| Non-epithelial | Stage I/II | Intermediate-delay | 1.01(0.50,2.04) | 0.977 | 0.80(0.31,2.04) | 0.636 |
| Long-delay | 1.20(0.28,5.17) | 0.802 | 1.54(0.33,7.11) | 0.582 | ||
| Stage III/IV | Intermediate-delay | 1.31(0.95,1.82) | 0.104 | 1.49(1.03,2.16) | 0.032 | |
| Long-delay | 0.71(0.35,1.44) | 0.342 | 0.87(0.39,1.93) | 0.732 | ||
HRa: compared with immediate-treatment initiation
HRb: compared with immediate-treatment initiation
Subgroupc: immediate: < 1 month, intermediate-delay: 1-2 months, and long-delay: ≥3 months
Our study assessed the impact of treatment interval on the prognosis of ovarian cancer using data from a national population-based database; we found that delayed treatment was an independent risk factor for ovarian cancer prognosis. The 5-year probability of OS was 61.4% in the immediate-treatment group, while it decreased sharply to 36.4% and 34.8% in the intermediate- and long-delay groups, respectively. Similarly, the 5-year CSS also showed a downward trend when switching between the three groups, with rates of 66.7%, 42.6% and 41.8%, respectively. In the multifactorial Cox analysis, the mortality risks of OS and CSS were higher in the intermediate-delay group than in the immediate-treatment group. Similarly, elevated risk values for OS and CSS were observed in the long-delay group; however, no statistically significant results could be calculated owing to the small sample size of this cohort. In summary, our study shows that patients with ovarian cancer are at an increased risk of mortality if their treatment is delayed for over 1 month since diagnosis. Several studies have reported the adverse effects of delayed treatment on the prognosis of patients with breast, liver, and colorectal tumors, and our results are consistent with these findings [11, 18-21]. An analysis by Hanna et al. [22] of seven types of cancers revealed that the mortality risk increases by 6-8% for every month surgery is postponed. Minami et al. [23] found that delayed surgical treatment slightly affected the pathological staging of patients with ductal carcinoma in situ but did not affect OS. Another study suggests that delay has the least effect on sub-centimeter nodules and may have the greatest effect on stage II disease [24]. We speculate that such an effect of delay is related to clinical characteristics and disease stage.
Forest plots for subgroup analysis of OS. HR1 P1 HR of the intermediate-delay group compared with that of the immediate treatment group. HR2 P2 HR of the long-delay group compared with that of the immediate treatment group.
Forest plots for subgroup analysis of CSS. HR1 P1 HR of the intermediate-delay group compared with that of the immediate treatment group. HR2 P2 HR of the long-delay group compared with that of the immediate treatment group.
There is a correlation between age and treatment delay, and similar observations have been made in other studies, showing that treatment refusal rates increase with age among patients with cancer [25]. There are also racial and ethnic differences in treatment delays [20]. Black patients have a higher probability of delaying initial surgery and chemotherapy treatment [26-28], which may be associated with specific social factors and, ultimately, lead to an increased risk of death [29, 30]. Marital status has also been associated with treatment delay, with married patients having shorter waiting intervals from diagnosis to treatment [10]. This may be related to the psychosocial support and economic support of their spouse, leading to more aggressive visits to the hospital to actively seek help and cooperate to undergo early treatment.
The histology and stage are important factors affecting the prognosis of patients with ovarian cancer; therefore, we performed a stratified analysis based on these two factors. We found that delays in treatment significantly impaired the prognosis of patients with serous tumors and stage I/II clear cell tumors. In further stratified analysis according both demographic and clinical characteristics, we found that patients aged <60 years, who are black, are in stage I/II, with epithelial tumors and not receiving chemotherapy and/or surgery are more clinically beneficial if treated immediately. If these patients underwent intermediate-delay treatment, the risk of death would be increased relative to other subgroups of patients. The results suggest the importance of early and aggressive intervention as clinicians can standardize the time window for patients who must wait for treatment based on these results and manage these patients more promptly. In addition, prehabilitation can improves tolerance during surgery and chemotherapy [10], women with advanced disease, advanced age, and comorbidities who are unable to tolerate major upfront surgery may be able to delay surgery by undergoing prehabilitation prior to surgery.
Ovarian cancer has the lowest 5-year survival rate among all gynecological tumors. The current mainstream treatment paradigm is dedicated to the development of novel therapeutic approaches. The implications of the results of our study are that, if the time window for the initial treatment of ovarian cancer is reduced to within 1 month, survival optimization may be achieved. This evidence also has important socioeconomic value, as gains in improved survival from shortening the time between diagnosis and initiation of treatment may be comparable to or greater than the benefits of developing some of the novel therapeutic agents [31, 32].
The present study had some limitations. First, there were potential confounding factors and selective bias in the data processing. Second, we currently have limited information on delayed treatment. Limitations of the SEER database prevented us from collecting specific patterns of initial treatment related to the time interval from diagnosis to treatment. Third, the long-term delayed treatment group had fewer patients and low statistical testing power, so the generalisation of the conclusions remains cautious. Finally, the SEER database is based on data from US registries, and it is unclear whether the results are applicable to other countries or regions.
Conclusions
Our study shows that prolonged initial treatment time is associated with poor prognosis in ovarian cancer patients. We recommend that ovarian cancer be treated within 1 month of diagnosis. Still, causality should be taken with caution, given the source of the data and the vast factors affecting treatment delays and prognosis in ovarian cancer. Gynecological oncologists should be aware of the impact of delayed treatment on the subsequent survival of patients with ovarian cancer and ensure timely treatment of patients after diagnosis to improve patient survival outcomes.
Abbreviations
CA 125: cancer antigen 125; CI: confidence interval; COVID-19: coronavirus disease 2019; CSS: cancer-specific survival; HR: hazard ratio; ICD-O-3: International Classification of Oncological Diseases 3; IQR: interquartile range; NACT: neoadjuvant chemotherapy; OS: overall survival; SEER: Surveillance, Epidemiology, and End Results.
Acknowledgements
We would like to thank the SEER database for providing the data for the statistical study.
Funding
This work was supported by National Natural Science Foundation of China (82272778), Innovation Program of Shanghai Science and Technology Committee (20Y11914200).
Availability of data
Relevant study data can be extracted from the SEER database using the software: SEER*Stat (https://seer.cancer.gov/seerstat/).
Ethical approval statement
The study was waived by the Ethics Review Committee of the Shanghai First Maternity and Infant Hospital due to the retrospective analysis of the database data used.
Author contributions
JZ performed the data analysis and wrote the first draft of the article, RC performed the data collection, YZ performed the additional data collection, HZ and YW designed study and revised the article. All authors read and approved the final manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA: a cancer journal for clinicians. 2022;72:7-33
2. Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD. et al. Ovarian cancer statistics, 2018. CA: a cancer journal for clinicians. 2018;68:284-96
3. Hou YM, Xue Y, Yao JM, Feng F, An RF. Relationship Between Neoadjuvant Chemotherapy and Log Odds of Positive Lymph Nodes and Their Prognostic Role in Advanced Ovarian Cancer Patients with Optimal Cytoreductive Surgery. Frontiers in oncology. 2022;12:878275
4. Hermens M, van Altena AM, van der Aa M, Bulten J, van Vliet H, Siebers AG. et al. Ovarian cancer prognosis in women with endometriosis: a retrospective nationwide cohort study of 32,419 women. American journal of obstetrics and gynecology. 2021;224:284.e1-e10
5. Urban RR, He H, Alfonso R, Hardesty MM, Gray HJ, Goff BA. Ovarian cancer outcomes: Predictors of early death. Gynecologic oncology. 2016;140:474-80
6. Cress RD, Chen YS, Morris CR, Petersen M, Leiserowitz GS. Characteristics of Long-Term Survivors of Epithelial Ovarian Cancer. Obstetrics and gynecology. 2015;126:491-7
7. Neal RD, Allgar VL, Ali N, Leese B, Heywood P, Proctor G. et al. Stage, survival and delays in lung, colorectal, prostate and ovarian cancer: comparison between diagnostic routes. The British journal of general practice: the journal of the Royal College of General Practitioners. 2007;57:212-9
8. Pyeon SY, Han GH, Ki KD, Lee KB, Lee JM. Effect of delayed palliative chemotherapy on survival of patients with recurrent ovarian cancer. PloS one. 2020;15:e0236244
9. Yi Q, Ran Y, Li C. The Effect of Delayed Chemotherapy on the Decrease of CA125 in Epithelial Ovarian Cancer During Coronavirus Disease Pandemic in 2020. Cancer management and research. 2021;13:515-20
10. Min Y, Liu Z, Huang R, Li R, Jin J, Wei Z. et al. Survival outcomes following treatment delays among patients with early-stage female cancers: a nationwide study. Journal of translational medicine. 2022;20:560
11. Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN. et al. Time to Surgery and Breast Cancer Survival in the United States. JAMA oncology. 2016;2:330-9
12. Chen CP, Kung PT, Wang YH, Tsai WC. Effect of time interval from diagnosis to treatment for cervical cancer on survival: A nationwide cohort study. PloS one. 2019;14:e0221946
13. Nagle CM, Francis JE, Nelson AE, Zorbas H, Luxford K, de Fazio A. et al. Reducing time to diagnosis does not improve outcomes for women with symptomatic ovarian cancer: a report from the Australian Ovarian Cancer Study Group. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29:2253-8
14. Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J. et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. British journal of cancer. 2015;112(Suppl 1):S92-107
15. Noer MC, Sperling CD, Ottesen B, Antonsen SL, Christensen IJ, Høgdall C. Ovarian Cancer and Comorbidity: Is Poor Survival Explained by Choice of Primary Treatment or System Delay? International journal of gynecological cancer: official journal of the International Gynecological Cancer Society. 2017;27:1123-33
16. Sud A, Jones ME, Broggio J, Loveday C, Torr B, Garrett A. et al. Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Annals of oncology: official journal of the European Society for Medical Oncology. 2020;31:1065-74
17. He S, Wang Y, Zhao X, Xu F, Li J, Huang T. et al. Factors Influencing Delayed Treatment in Patients with Breast Cancer During COVID-19 Pandemic. Frontiers in public health. 2022;10:808873
18. Eaglehouse YL, Georg MW, Shriver CD, Zhu K. Time-to-surgery and overall survival after breast cancer diagnosis in a universal health system. Breast cancer research and treatment. 2019;178:441-50
19. Corley DA, Jensen CD, Quinn VP, Doubeni CA, Zauber AG, Lee JK. et al. Association Between Time to Colonoscopy After a Positive Fecal Test Result and Risk of Colorectal Cancer and Cancer Stage at Diagnosis. Jama. 2017;317:1631-41
20. Wagle NS, Park S, Washburn D, Ohsfeldt RL, Rich NE, Singal AG. et al. Racial, Ethnic, and Socioeconomic Disparities in Treatment Delay Among Patients with Hepatocellular Carcinoma in the United States. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association. 2022
21. Elit LM, O'Leary EM, Pond GR, Seow HY. Impact of wait times on survival for women with uterine cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2014;32:27-33
22. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, Harvey-Jones E. et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ (Clinical research ed). 2020;371:m4087
23. Minami CA, Kantor O, Weiss A, Nakhlis F, King TA, Mittendorf EA. Association Between Time to Operation and Pathologic Stage in Ductal Carcinoma in Situ and Early-Stage Hormone Receptor-Positive Breast Cancer. Journal of the American College of Surgeons. 2020;231:434-47.e2
24. Zuniga PVS, Ost DE. Impact of Delays in Lung Cancer Treatment on Survival. Chest. 2021;160:1934-58
25. Noh KW, Kim B, Choi CH, Kim TJ, Lee JW, Kim BG. et al. Effect of Waiting Time from Pathological Diagnosis to Definitive Concurrent Chemoradiation for Cervical Cancer on Overall Survival. Cancer research and treatment. 2022;54:245-52
26. McGee SA, Durham DD, Tse CK, Millikan RC. Determinants of breast cancer treatment delay differ for African American and White women. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22:1227-38
27. Livaudais JC, Hershman DL, Habel L, Kushi L, Gomez SL, Li CI. et al. Racial/ethnic differences in initiation of adjuvant hormonal therapy among women with hormone receptor-positive breast cancer. Breast cancer research and treatment. 2012;131:607-17
28. Wu J, Sun H, Yang L, Deng Y, Yan Y, Wang S. et al. Improved survival in ovarian cancer, with widening survival gaps of races and socioeconomic status: a period analysis, 1983-2012. Journal of Cancer. 2018;9:3548-56
29. Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI. Delay in initiating adjuvant radiotherapy following breast conservation surgery and its impact on survival. International journal of radiation oncology, biology, physics. 2006;65:1353-60
30. Bikomeye JC, Zhou Y, McGinley EL, Canales B, Yen TWF, Tarima S. et al. Historical Redlining and Breast Cancer Treatment and Survival among older Women in the US. Journal of the National Cancer Institute. 2023
31. Davis C, Naci H, Gurpinar E, Poplavska E, Pinto A, Aggarwal A. Availability of evidence of benefits on overall survival and quality of life of cancer drugs approved by European Medicines Agency: retrospective cohort study of drug approvals 2009-13. BMJ (Clinical research ed). 2017;359:j4530
32. Dottino JA, Cliby WA, Myers ER, Bristow RE, Havrilesky LJ. Improving NCCN guideline-adherent care for ovarian cancer: Value of an intervention. Gynecologic oncology. 2015;138:694-9
Author contact
![]() Corresponding authors: Yu Wang, Department of Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, No. 2699 Gaokexi Road, Shanghai 200092, China; Email: renjiwangyucom. Haiyan Zhu, Department of Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, No. 2699 Gaokexi Road, Shanghai 200092, China; Email: zhuhaiyandoccom.
Corresponding authors: Yu Wang, Department of Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, No. 2699 Gaokexi Road, Shanghai 200092, China; Email: renjiwangyucom. Haiyan Zhu, Department of Shanghai Key Laboratory of Maternal Fetal Medicine, Shanghai Institute of Maternal-Fetal Medicine and Gynecologic Oncology, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, No. 2699 Gaokexi Road, Shanghai 200092, China; Email: zhuhaiyandoccom.

 Global reach, higher impact
Global reach, higher impact