Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(2):484-493. doi:10.7150/jca.90128 This issue Cite
Review
Predictive Biomarkers of Immune Checkpoint Inhibitor-Based Mono- and Combination Therapies for Hepatocellular Carcinoma
1. Organ Transplantation Center, China Medical University Hospital, Taichung, Taiwan.
2. Department of Surgery, China Medical University Hospital, Taichung, Taiwan.
3. Cell Therapy Center, China Medical University Hospital, Taichung, Taiwan.
4. Department of Pathology, China Medical University Hospital, Taichung, Taiwan.
5. Graduate Institute of Biomedical Sciences, China Medical University, Taichung, Taiwan.
6. Program for Cancer Biology and Drug Development, China Medical University, Taichung, Taiwan.
7. Research Center for Cancer Biology, China Medical University, Taichung, Taiwan.
Received 2023-9-13; Accepted 2023-11-12; Published 2024-1-1
Abstract
Hepatocellular carcinoma (HCC) is among the most frequent and deadly human cancers worldwide. It has been shown that interaction between immune checkpoint receptors and ligands plays a crucial role in inhibition of T cell-mediated anti-tumor immune responses, thereby assisting tumor cells to evade the host immune surveillance. Therefore, several immune checkpoint inhibitors (ICIs) that selectively block immune checkpoint receptors or ligands have been developed as clinically effective and safe immunotherapeutic agents for treating HCC, including the inhibitors targeting cytotoxic T lymphocyte-associated antigen 4, programmed death 1, and programmed death ligand 1. In addition, various combinations of ICIs and other ICIs or tyrosine kinase inhibitors or vascular endothelial growth factor inhibitors have also emerged as clinically beneficial treatments for HCC. However, the overall response rates of ICI mono-therapy and combination therapy in HCC patients remain unsatisfied, highlighting the urgent need for discovering valuable predictive biomarkers to achieve personalized therapy. This review comprehensively summarizes the literature-based evidence validating a variety of biomarkers with predictive significance for treatment responses and outcomes in HCC patients receiving various ICI-based mono- and combination therapies.
Keywords: hepatocellular carcinoma, immune checkpoint inhibitor, mono-therapy, combination therapy, predictive biomarker
Introduction
As the predominant type of primary liver cancer, hepatocellular carcinoma (HCC) accounts for over 90% of primary liver malignancies and is the sixth most prevalent and the third most deadly human cancer worldwide, contributing to approximately 900,000 cases and 800,000 deaths per year [1-3]. Many therapeutic options have been well established for treating HCC, including surgical therapies (such as liver transplantation and resection) [4, 5], locoregional therapies (such as radiotherapy, ablation, and embolization) [6, 7], and systemic therapies (such as chemotherapy and molecular targeted therapy) [8, 9]. Moreover, immunotherapies such as immune checkpoint inhibitor (ICI) therapy have been developed as a promising treatment modality for HCC [10, 11]. However, the therapeutic efficacy of these treatment modalities varies among patients and remains to be improved. Therefore, the discovery of valuable biomarkers for predicting therapeutic responses and outcomes in HCC patients is an important goal to select the most suitable patient for the most suitable treatment (the so-called personalized therapy) to improve patient survival.
Immune checkpoint molecules include the co-inhibitory receptors expressed by effector T cells and the corresponding ligands expressed by tumor cells and stromal cells [12, 13]. Through the interaction between the receptors and ligands, immune checkpoint molecules play an important role in suppression of the activation and function of effector T cells, thereby facilitating tumor cell escape from T cell-mediated anti-tumor immune responses [14, 15]. As a result, many monoclonal antibodies that block the binding of immune checkpoint receptors to ligands (the so-called ICIs) have been generated as effective immunotherapeutic agents to restore T cell-mediated killing of tumor cells [16, 17]. The ICIs that have been licensed or are in clinical research for HCC treatment include the agents targeting the co-inhibitory receptors such as cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and programmed death 1 (PD-1) and the agents targeting the ligand of PD-1, programmed death ligand 1 (PD-L1) [18-20]. In addition, the combination of ICIs targeting CTLA-4 and PD-1 or PD-L1, the combination of ICIs targeting PD-1 or PD-L1 and tyrosine kinase inhibitors (TKIs), and the combination of ICIs targeting PD-L1 and vascular endothelial growth factor (VEGF) inhibitors have been also licensed or are under clinical validation for HCC therapy [18-20]. It has been shown that ICI-based mono- and combination therapies are active, tolerate, and clinically beneficial against HCC, although patients may concurrently receive various locoregional therapies. However, the overall response rates remain unsatisfied in HCC patients, with only about 15% and 30% for ICI-based mono- and combination therapies, respectively [18-20]. Therefore, the development of clinically useful predictive biomarkers for identifying HCC patients who are more likely to respond to ICIs is urgently needed to advance personalized therapy for better patient outcomes.
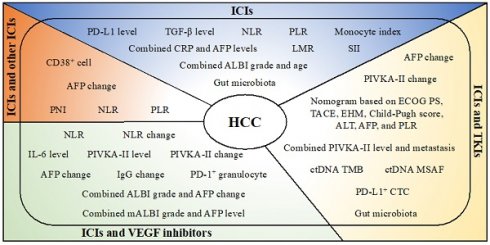
This review provides a comprehensive summary of the hitherto published literature, which unravel various promising biomarkers at pre-treatment, on-treatment, and post-treatment time points in tissue, blood, and stool samples for predicting the therapeutic responses and clinical benefits of different categories of ICI-based therapies in HCC patients, including ICI mono-therapy and combination therapy with other ICIs or TKIs or VEGF inhibitors.
Predictive biomarkers of ICI mono-therapy for HCC
Several biomarkers have been validated with predictive value in HCC patients receiving ICI mono-therapy in multiple lines of studies (Table 1). The study conducted by Sangro et al. [21] analyzed the pre-treatment expression of PD-L1 in tumor tissues of 195 HCC patients treated with PD-1 ICI (nivolumab) and showed that high PD-L1 expression level (≥ 1%) was associated with better median overall survival (OS) (28.1 versus (vs.) 16.6 months, P value = 0.03) than low PD-L1 expression level (< 1%). The study conducted by Feun et al. [22] evaluated the pre-treatment levels of a panel of cytokines and chemokines in blood of 28 HCC patients treated with PD-1 ICI (pembrolizumab) and identified that low transforming growth factor-beta (TGF-β) level (< 200 pg/mL) predicted longer median OS (not reached (NR) vs. 7 months, P value = 0.005) and progression-free survival (PFS) (NR vs. 2 months, P value = 0.008) than high TGF-β level (≥ 200 pg/mL). The study conducted by Zhang et al. [23] combined the pre-treatment blood levels of C-reactive protein (CRP) and alpha-fetoprotein (AFP) to stratify 101 HCC patients treated with PD-1 ICI (such as nivolumab, toripalimab, sintilimab, and pembrolizumab) into low-risk (CRP ≤ 20.9 mg/L and AFP ≤ 400 ng/mL), medium-risk (CRP > 20.9 mg/L or AFP > 400 ng/mL), and high-risk (CRP > 20.9 mg/L and AFP > 400 ng/mL) subgroups and confirmed that patients with a low-risk score had the highest disease control rate (DCR) (82% vs. 65% vs. 35%, P value = 0.002) and the best OS (P value < 0.001) and PFS (P value < 0.001) compared with patients with a medium- or high-risk score. The study conducted by Dong et al. [24] combined the pre-treatment albumin-bilirubin (ALBI) grade and age to stratify 38 HCC patients treated with PD-1 ICI (such as sintilimab and camrelizumab) combined with locoregional therapy (such as conventional radiotherapy (CRT), hypofractionated radiotherapy (HFRT), and stereotactic body radiotherapy (SBRT)) into low-risk (ALBI grade 1 and age ≥ 53 years) and high-risk (ALBI grade 2 and age < 53 years) subgroups and revealed that patients with a low-risk score had higher objective response rate (ORR) (50% vs. 14%, P value = 0.001) and longer median OS (NR vs. 10.1 months, P value = 0.003) and PFS (15.3 vs. 2.7 months, P value < 0.001) than patients with a high-risk score. In addition, the study conducted by Choi et al. [25] measured the pre-treatment counts of neutrophils and lymphocytes in blood of 194 HCC patients treated with PD-1 ICI (nivolumab) and indicated that low neutrophil to lymphocyte ratio (NLR) (< 3) was correlated with longer median OS (61.3 vs. 21.0 weeks, P value < 0.001) and PFS (11.0 vs. 7.1 weeks, P value = 0.01) than high NLR (≥ 3). The study conducted by Hung et al. [26] also calculated the NLR in blood of 45 HCC patients treated with PD-1 ICI (nivolumab) and verified that low pre-treatment NLR (≤ 2.5), on-treatment NLR (< 4.1), or post-treatment NLR (≤ 2.7) predicted DCR (sensitivity/specificity, 57%/97%; 86%/58%; 64%/87%, respectively) and longer PFS (P value = 0.004; P value = 0.006; P value = 0.001, respectively) than high pre-treatment NLR (> 2.5), on-treatment NLR (≥ 4.1), or post-treatment NLR (> 2.7). The study conducted by Dharmapuri et al. [27] detected both NLR and platelet to lymphocyte ratio (PLR) in blood of 103 HCC patients treated with PD-1 ICI (nivolumab) combined with or without locoregional therapy (such as transarterial chemoembolization (TACE) and transarterial radioembolization (TARE)) and showed that low pre-treatment or post-treatment NLR (all < 5) predicted longer median OS (23 vs. 10 months, P value = 0.004; 35 vs. 9 months, P value < 0.001, respectively) and PFS (16 vs. 5 months, P value = 0.022; 35 vs. 5 months, P value < 0.001, respectively) than high NLR (≥ 5). When PLR was divided into low (≤ 118 for pre-treatment; ≤ 125 for post-treatment), medium (> 118 to < 224 for pre-treatment; > 125 to < 229 for post-treatment), and high (≥ 224 for pre-treatment; ≥ 229 for post-treatment) level groups, patients with a low pre-treatment or post-treatment PLR had the longest median OS (35 vs. 10 vs. 15 months, P value = 0.05; NR vs. 19 vs. 10 months, P value = 0.013, respectively) compared with patients with a medium or high PLR. The study conducted by Huang et al. [28] determined the pre-treatment NLR, PLR, systemic immune-inflammation index (SII), and lymphocyte to monocyte ratio (LMR) in blood of 110 HBV-related HCC patients treated with PD-1 ICI and demonstrated that low NLR (< 5), PLR (< 140), or SII (< 970) or high LMR (≥ 1.8) was associated with longer median OS (7.3 vs. 6.0 months, P value = 0.0007; 7.3 vs. 6.7 months, P value = 0.0029; 7.2 vs. 5.9 months, P value < 0.0001; 7.2 vs. 6.7 months, P value = 0.0038, respectively) and PFS (6.7 vs. 5.4 months, P value = 0.0013; 6.7 vs. 5.9 months, P value = 0.0016; 6.7 vs. 4.5 months, P value < 0.0001; 6.8 vs. 5.5 months, P value = 0.0006, respectively) than high NLR (≥ 5), PLR (≥ 140), or SII (≥ 970) or low LMR (< 1.8). The study conducted by Jeon et al. [29] measured the frequency of classical monocytes (cMonocyte) and PD-L1-expressing classical monocytes (cMonocyte-PDL1) in blood of 45 HCC patients treated with PD-1 ICI (nivolumab) and calculated the on-treatment monocyte index by dividing cMonocyteD7/D0 by cMonocyte-PDL1D7/D0, in which cMonocyteD7/D0 and cMonocyte-PDL1D7/D0 were defined as the fold change in the frequency of cMonocyte and cMonocyte-PDL1 at day 7 over day 0 after treatment initiation, respectively. It was shown that high monocyte index (≥ 1) predicted DCR (sensitivity/specificity, 83%/65%) and better PFS (P value = 0.008) than low monocyte index (< 1). Moreover, the study conducted by Mao et al. [30] analyzed the pre-treatment composition of gut microbiota in stool of 30 HCC patients treated with PD-1 ICI and ascertained that patients with a high abundance of Erysipelotrichaceae bacterium-GAM79 or low abundance of Veillonellaceae had longer median OS (NR vs. 15.9 months, P value = 0.041; NR vs. 7.8 months, P value = 0.03, respectively) and PFS (15.9 vs. 5.5 months, P value = 0.021; 10.8 vs. 3.6 months, P value = 0.005, respectively) than patients with a low abundance of Erysipelotrichaceae bacterium-GAM79 or high abundance of Veillonellaceae.
Predictive biomarkers of ICI mono-therapy for HCC
| Biomarkers | Source | Patients and Treatment | Predictive Significancea | Year | References |
|---|---|---|---|---|---|
| Pre-treatment tumoral PD-L1 expression levelb | Tissue | 195 HCC patients treated with PD-1 ICI | High PD-L1 expression level predicted longer OS. | 2020 | Sangro et al. [21] |
| Pre-treatment TGF-β levelc | Blood | 28 HCC patients treated with PD-1 ICI | Low TGF-β level predicted longer OS and PFS. | 2019 | Feun et al. [22] |
| Pre-treatment CRP and AFP levelsd | Blood | 101 HCC patients treated with PD-1 ICI | Patients with a low-risk score had the highest DCR and the longest OS and PFS, followed by patients with a medium- or high-risk score. | 2022 | Zhang et al. [23] |
| Pre-treatment ALBI grade and agee | Blood | 38 HCC patients treated with PD-1 ICI combined with locoregional therapy | Patients with a low-risk score had higher ORR and longer OS and PFS than patients with a high-risk score. | 2022 | Dong et al. [24] |
| Pre-treatment NLRf | Blood | 194 HCC patients treated with PD-1 ICI | Low NLR predicted longer OS and PFS. | 2021 | Choi et al. [25] |
| Pre-treatment, on-treatment, or post-treatment NLRg | Blood | 45 HCC patients treated with PD-1 ICI | Low pre-treatment, on-treatment, or post-treatment NLR predicted DCR and longer PFS. | 2021 | Hung et al. [26] |
| Pre-treatment or post-treatment NLR or PLRh | Blood | 103 HCC patients treated with PD-1 ICI combined with or without locoregional therapy | Low pre-treatment or post-treatment NLR predicted longer OS and PFS. Patients with a low pre-treatment or post-treatment PLR had the longest OS, followed by patients with a medium or high PLR. | 2020 | Dharmapuri et al. [27] |
| Pre-treatment NLR, PLR, SII, or LMRi | Blood | 110 HBV-related HCC patients treated with PD-1 ICI | Low NLR, PLR, or SII, or high LMR predicted longer OS and PFS. | 2022 | Huang et al. [28] |
| On-treatment monocyte indexj | Blood | 45 HCC patients treated with PD-1 ICI | High monocyte index predicted DCR and longer PFS. | 2023 | Jeon et al. [29] |
| Pre-treatment gut microbiota | Stool | 30 HCC patients treated with PD-1 ICI | High abundance of Erysipelotrichaceae bacterium-GAM79 or low abundance of Veillonellaceae predicted longer OS. | 2021 | Mao et al. [30] |
aOS was defined as the time from treatment initiation to death due to any cause. PFS was defined as the time from treatment initiation to radiological progression or death due to any cause. ORR was defined as the proportion of patients with CR or PR. DCR was defined as the proportion of patients with CR, PR, or SD.
bTumoral PD-L1 expression was defined as the percentage of PD-L1-expressing tumor cells in tumor tissues and was categorized as high (≥ 1%) or low (< 1%) level.
cTGF-β level was categorized as high (≥ 200 pg/mL) or low (< 200 pg/mL) level.
dThe combination of CRP and AFP levels was categorized as high (CRP > 20.9 mg/L and AFP > 400 ng/mL), medium (CRP > 20.9 mg/L or AFP > 400 ng/mL), or low (CRP ≤ 20.9 mg/L and AFP ≤ 400 ng/mL) risk.
eALBI grade was defined as log10 blood bilirubin level multiplied by 0.66 plus blood albumin level multiplied by -0.085 and was stratified as grade 1 (≤ -2.60), 2 (> -2.60 to ≤ -1.39), or 3 (> -1.39). The combination of ALBI grade and age was categorized as high (ALBI grade 2 and age < 53 years) or low (ALBI grade 1 and age ≥ 53 years) risk.
fNLR was calculated by dividing blood neutrophil count by blood lymphocyte count and was categorized as high (≥ 3) or low (< 3) ratio.
gOn-treatment NLR was measured at day 14 after treatment initiation. Pre-treatment, on-treatment, and post-treatment NLR were categorized as high (> 2.5, ≤ 4.1, and > 2.7) or low (≤ 2.5, < 4.1, and ≤ 2.7) ratio, respectively.
hNLR was categorized as high (≥ 5) or low (< 5) ratio for pre-treatment and post-treatment. PLR was calculated by dividing blood platelet count by blood lymphocyte count and was divided into three level groups: low (≤ 118), medium (> 118 to < 224), and high (≥ 224) for pre-treatment; low (≤ 125), medium (> 125 to < 229), and high (≥ 229) for post-treatment.
iNLR was categorized as high (≥ 5) or low (< 5) ratio. PLR was categorized as high (≥ 140) or low (< 140) ratio. SII was calculated by multiplying blood platelet count by blood neutrophil count and dividing by blood lymphocyte count and was categorized as high (≥ 970) or low (< 970) index. LMR was calculated by dividing blood lymphocyte count by blood monocyte count and was categorized as high (≥ 1.8) or low (< 1.8) ratio.
jMonocyte index was calculated by dividing MonocyteD7/D0 by Monocyte-PDL1D7/D0, in which MonocyteD7/D0 was defined as the fold change in the frequency of classical monocytes at day 7 over day 0 after treatment initiation and Monocyte-PDL1D7/D0 was defined as the fold change in the frequency of PD-L1-expressing classical monocytes at day 7 over day 0 after treatment initiation in blood, and was categorized as high (≥ 1) or low (< 1) index.
Abbreviations: ICI, immune checkpoint inhibitor; HCC, hepatocellular carcinoma; PD-L1, programmed death ligand 1; PD-1, programmed death 1; OS, overall survival; TGF-β, transforming growth factor-beta; PFS, progression-free survival; CRP, C-reactive protein; AFP, alpha-fetoprotein; DCR, disease control rate; ALBI, albumin-bilirubin; ORR, objective response rate; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; SII, systemic immune-inflammation index; LMR, lymphocyte to monocyte ratio; HBV, hepatitis B virus; CR, complete response; PR, partial response; SD, stable disease.
Predictive biomarkers of ICI combination therapy with other ICIs or TKIs for HCC
The predictive value of many biomarkers in HCC patients receiving ICI combination therapy with other ICIs or TKIs have been validated in multiple lines of studies (Table 2). The study conducted by Ng et al. [31] investigated the pre-treatment expression of CD38 in tumor tissues of 49 HCC patients treated with PD-1 or PD-L1 ICI combined with or without CTLA-4 ICI and showed that high CD38-positive (CD38+) cell proportion (≥ 5%) was associated with higher ORR (43% vs. 4%, P value = 0.019) and longer median OS (19.1 vs. 9.6 months, P value = 0.0295) and PFS (8.2 vs. 1.6 months, P value = 0.0065) than low CD38+ cell proportion (< 5%). The study conducted by Muhammed et al. [32] measured the pre-treatment prognostic nutritional index (PNI), NLR, and PLR in blood of 362 HCC patients treated with PD-1 ICI (such as nivolumab and pembrolizumab) or PD-L1 ICI (such as atezolizumab, avelumab, and durvalumab) combined with or without CTLA-4 ICI (ipilimumab) and revealed that high PNI (≥ 45) predicted higher DCR (66% vs. 52%, P value = 0.014) and longer median OS (17.7 vs. 10.8 months, P value = 0.018) than low PNI (< 45); low NLR (< 5) predicted higher ORR (22% vs. 12%, P value = 0.034) and longer median OS (17.6 vs. 7.7 months, P value = 0.0001) and PFS (3.8 vs. 2.1 months, P value = 0.025) than high NLR (≥ 5); low PLR (< 300) predicted longer median OS (16.5 vs. 6.4 months, P value < 0.0001) and PFS (3.7 vs. 1.8 months, P value = 0.0006) than high PLR (≥ 300). In addition, the study conducted by Shao et al. [33] detected the on-treatment change in AFP levels in blood of 43 HCC patients treated with PD-1 ICI combined with or without CTLA-4 ICI and identified that high AFP decrease (> 20%) predicted higher ORR (73% vs. 14%, P value < 0.001) and DCR (80% vs. 46%, P value = 0.033) and longer median OS (28.0 vs. 11.2 months, P value = 0.048) and PFS (15.2 vs. 2.7 months, P value = 0.002) than low AFP decrease (≤ 20%). The studies conducted by Lee et al. [34] and Hsu et al. [35] also evaluated the on-treatment AFP change in blood of patients. The former study confirmed that high AFP decrease (> 10%) predicted higher ORR (64% vs. 10%, P value < 0.001) and DCR (82% vs. 14%, P value < 0.001) and longer median OS (24.7 vs. 6.9 months, P value = 0.009) than low AFP decrease (≤ 10%) in 75 HCC patients treated with PD-1 ICI (such as nivolumab and pembrolizumab) combined with or without TKI (such as sorafenib, regorafenib, and lenvatinib); the latter study verified that high AFP decrease (> 15%) predicted higher ORR (46% vs. 10%, P value < 0.001) and DCR (80% vs. 29%, P value < 0.001) and longer median OS (21.9 vs. 5.6 months, P value < 0.001) and PFS (7.5 vs. 2.3 months, P value < 0.001) than low AFP decrease (≤ 15%) in 95 HCC patients treated with PD-1 ICI (such as nivolumab and pembrolizumab) combined with or without locoregional therapy (such as SBRT, TACE, and radiofrequency ablation (RFA)) or TKI (such as sorafenib, regorafenib, and lenvatinib). The study conducted by Sun et al. [36] analyzed the post-treatment change in AFP and protein induced by vitamin K absence or antagonist-II (PIVKA-II) levels in blood of 235 HCC patients treated with PD-1 ICI (such as nivolumab, toripalimab, sintilimab, camrelizumab, and pembrolizumab) combined with or without locoregional therapy (TACE) and/or TKI and demonstrated that high AFP decrease (> 50%) or PIVKA-II decrease (> 50%) was correlated with higher ORR (53% vs. 18%, P value < 0.001; 50% vs. 18%, P value = 0.003, respectively) and longer median OS (NR vs. 13.7 months, P value = 0.003; NR vs. 14.4 months, P value = 0.006, respectively) and PFS (13.1 vs. 4.5 months, P value < 0.001; 10.9 vs. 4.5 months, P value = 0.021, respectively) than low AFP decrease (≤ 50%) or PIVKA-II decrease (≤ 50%). The study conducted by Li et al. [37] established a nomogram based on 7 pre-treatment clinical parameters including Eastern Cooperative Oncology Group performance status (ECOG PS), TACE, extrahepatic metastasis (EHM), Child-Pugh score, alanine aminotransferase (ALT), AFP, and PLR to stratify 258 HCC patients treated with PD-1 ICI (such as sintilimab and camrelizumab) combined with or without TKI (such as sorafenib, regorafenib, and lenvatinib) and ascertained that patients with a low-risk score (≤ 182.7) had the longest median OS (53.2 vs. 17.5 vs. 7.6 months, P value < 0.0001) compared with patients with a medium-risk (> 182.7 to ≤ 240.3) or high-risk (> 240.3) score. The study conducted by Guo et al. [38] combined the pre-treatment PIVKA-II level and metastasis to stratify 191 HCC patients treated with PD-1 ICI (such as nivolumab, toripalimab, sintilimab, pembrolizumab, and tislelizumab) combined with TKI (lenvatinib) into low-risk (PIVKA-II < 600 mAU/mL and without metastasis), medium-risk (PIVKA-II > 600 mAU/mL or with metastasis), and high-risk (PIVKA-II > 600 mAU/mL and with metastasis) subgroups and found that patients with a low-risk score had the longest median OS (24.0 vs. 17.7 vs. 12.1 months, P value < 0.001) compared with patients with a medium- or high-risk score.
Predictive biomarkers of ICI combination therapy with other ICIs or TKIs for HCC
| Biomarkers | Source | Patients and Treatment | Predictive Significancea | Year | References |
|---|---|---|---|---|---|
| Pre-treatment intratumoral CD38+ cell proportionb | Tissue | 49 HCC patients treated with PD-1 or PD-L1 ICI combined with or without CTLA-4 ICI | High CD38+ cell proportion predicted higher ORR and longer OS and PFS. | 2020 | Ng et al. [31] |
| Pre-treatment PNI, NLR, or PLRc | Blood | 362 HCC patients treated with PD-1 or PD-L1 ICI combined with or without CTLA-4 ICI | High PNI predicted higher DCR and longer OS. Low NLR predicted higher ORR and longer OS and PFS. Low PLR predicted longer OS and PFS. | 2021 | Muhammed et al. [32] |
| On-treatment AFP changed | Blood | 43 HCC patients treated with PD-1 ICI combined with or without CTLA-4 ICI | High AFP decrease predicted higher ORR and DCR and longer OS and PFS. | 2019 | Shao et al. [33] |
| On-treatment AFP changee | Blood | 75 HCC patients treated with PD-1 ICI combined with or without TKI | High AFP decrease predicted higher ORR and DCR and longer OS. | 2020 | Lee et al. [34] |
| On-treatment AFP changef | Blood | 95 HCC patients treated with PD-1 ICI combined with or without locoregional therapy or TKI | High AFP decrease predicted higher ORR and DCR and longer OS and PFS. | 2021 | Hsu et al. [35] |
| Post-treatment AFP or PIVKA-II changeg | Blood | 235 HCC patients treated with PD-1 ICI combined with or without locoregional therapy and/or TKI | High AFP or PIVKA-II decrease predicted higher ORR and longer OS and PFS. | 2021 | Sun et al. [36] |
| Pre-treatment nomogram based on ECOG PS, TACE, EHM, Child-Pugh score, ALT, AFP, and PLRh | Blood | 258 HCC patients treated with PD-1 ICI combined with or without TKI | Patients with a low-risk score had the longest OS, followed by patients with a medium- or high-risk score. | 2022 | Li et al. [37] |
| Pre-treatment PIVKA-II level and metastasisi | Blood | 191 HCC patients treated with PD-1 ICI combined with TKI | Patients with a low-risk score had the longest OS, followed by patients with a medium- or high-risk score. | 2023 | Guo et al. [38] |
| Pre-treatment ctDNA TMB or MSAFj | Blood | 107 HCC patients treated with PD-1 ICI combined with TKI | Low ctDNA TMB predicted higher DCR and longer OS. Low ctDNA MSAF predicted higher DCR and longer OS. | 2022 | Xu et al. [39] |
| Pre-treatment PD-L1+ CTC countk | Blood | 47 HCC patients treated with PD-1 ICI combined with locoregional therapy and TKI | Low PD-L1+ CTC count predicted ORR and higher ORR and longer OS. | 2022 | Su et al. [40] |
| Pre-treatment gut microbiotal | Stool | 74 HCC patients treated with PD-1 ICI combined with or without TKI | Patients with a good signature of microbiota had the highest ORR and DCR and the longest OS and PFS, followed by patients with a fair or poor signature. | 2022 | Lee et al. [41] |
aOS was defined as the time from treatment initiation to death due to any cause. PFS was defined as the time from treatment initiation to radiological progression or death due to any cause. ORR was defined as the proportion of patients with CR or PR. DCR was defined as the proportion of patients with CR, PR, or SD.
bIntratumoral CD38+ cell proportion was defined as the percentage of CD38-expressing cells in tumor tissues and was categorized as high (≥ 5%) or low (< 5%) proportion.
cPNI was defined as blood albumin level plus 5 multiplies by blood lymphocyte count and was categorized as high (≥ 45) or low (< 45) index. NLR was calculated by dividing blood neutrophil count by blood lymphocyte count and was categorized as high (≥ 5) or low (< 5) ratio. PLR was calculated by dividing blood platelet count by blood lymphocyte count and was categorized as high (≥ 300) or low (< 300) ratio.
dAFP decrease was defined as the percentage of decrease in serum AFP levels at 4 weeks after treatment initiation relative to pre-treatment levels and was categorized as high (> 20%) or low (≤ 20%) decrease.
eAFP decrease was defined as the percentage of decrease in serum AFP levels at 4 weeks after treatment initiation relative to pre-treatment levels and was categorized as high (> 10%) or low (≤ 10%) decrease.
fAFP decrease was defined as the percentage of decrease in serum AFP levels at 3 months after treatment initiation relative to pre-treatment levels and was categorized as high (> 15%) or low (≤ 15%) decrease.
gAFP or PIVKA-II decrease was defined as the percentage of decrease in serum AFP or PIVKA-II levels after completion of treatment relative to pre-treatment levels and was categorized as high (> 50%) or low (≤ 50%) decrease.
hA total score was calculated based on the nomogram assigned ratio and was divided into three risk groups: low (≤ 182.7), medium (> 182.7 to ≤ 240.3), and high (> 240.3).
iThe combination of PIVKA-II level and metastasis was categorized as high (PIVKA-II > 600 mAU/mL and with metastasis), medium (PIVKA-II > 600 mAU/mL or with metastasis), or low (PIVKA-II < 600 mAU/mL and without metastasis) risk.
jTMB was defined as the number of somatic mutations per megabase of sequenced ctDNA and was categorized as high (> 4) or low (≤ 4) burden. MSAF is an indicator of the amount of ctDNA in blood and was categorized as high (> 0.027) or low (≤ 0.027) frequency.
kPD-L1+ CTC count was categorized as high (≥ 2) or low (< 2) count.
lGood signature was defined as the coexistence of Prevotella 9 depletion and Lachnoclostridium enrichment, poor signature was defined as the coexistence of Prevotella 9 enrichment and Lachnoclostridium depletion, and fair signature was defined as the coexistence of both two bacteria depletion or both two bacteria enrichment.
Abbreviations: ICI, immune checkpoint inhibitor; TKI, tyrosine kinase inhibitor; HCC, hepatocellular carcinoma; PD-1, programmed death 1; PD-L1, programmed death ligand 1; CTLA-4, cytotoxic T-lymphocyte associated antigen 4; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; PNI, prognostic nutritional index; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; DCR, disease control rate; AFP, alpha-fetoprotein; PIVKA-II, protein induced by vitamin K absence or antagonist-II; ECOG PS, Eastern Cooperative Oncology Group performance status; TACE, transarterial chemoembolization; EHM, extrahepatic metastasis; ALT, alanine aminotransferase; ctDNA, circulating tumor DNA; TMB, tumor mutation burden; MSAF, maximum somatic allele frequency; CTC, circulating tumor cell; CR, complete response; PR, partial response.
Moreover, the study conducted by Xu et al. [39] examined the pre-treatment levels of circulating tumor DNA (ctDNA) tumor mutation burden (TMB) and maximum somatic allele frequency (MSAF) in blood of 107 HCC patients treated with PD-1 ICI (camrelizumab) combined with TKI (apatinib). It was shown that low ctDNA TMB (≤ 4) predicted higher DCR (90% vs. 64%, P value = 0.002) and longer OS (P value = 0.019) than high ctDNA TMB (> 4); low ctDNA MSAF (≤ 0.027) predicted higher DCR (90% vs. 72%, P value = 0.043) and better OS (P value = 0.002) and PFS (P value = 0.004) than high ctDNA MSAF (> 0.027). The study conducted by Su et al. [40] determined the pre-treatment counts of PD-L1+ circulating tumor cells (CTCs) in blood of 47 HCC patients treated with PD-1 ICI (such as sintilimab, camrelizumab, and tislelizumab) combined with locoregional therapy (intensity-modulated radiotherapy (IMRT)) and TKI (such as sorafenib, regorafenib, lenvatinib, apatinib, and anlotinib) and unraveled that low PD-L1+ CTC count (< 2) predicted higher ORR (sensitivity/specificity, 77%/67%; 57% vs. 17%, P value = 0.007) and longer median OS (NR vs. 10.8 months, P value = 0.001) than high PD-L1+ CTC count (≥ 2). The study conducted by Lee et al. [41] monitored the pre-treatment composition of gut microbiota in stool of 74 HCC patients treated with PD-1 ICI (such as nivolumab and pembrolizumab) combined with or without TKI (41 patients as derivation cohort and 33 patients as validation cohort) and stratified patients into good-signature (coexistence of Prevotella 9 depletion and Lachnoclostridium enrichment), fair-signature (coexistence of both two bacteria depletion or both two bacteria enrichment), and poor-signature (coexistence of Prevotella 9 enrichment and Lachnoclostridium depletion) subgroups. In the derivation cohort, patients with a good-signature microbiota had the longest median OS (22.8 vs. 8.0 vs. 4.8 months, P value = 0.007) compared with patients with a fair- or poor-signature microbiota; in the validation cohort, patients with a good-signature microbiota had the highest ORR (53% vs. 20% vs. 0%, P value = 0.06) and DCR (95% vs. 90% vs. 0%, P value < 0.001) and the longest median OS (NR vs. 11.1 vs. 6.5 months, P value < 0.001) and PFS (8.8 vs. 7.6 vs. 1.8 months, P value < 0.001) compared with patients with a fair- or poor-signature microbiota.
Predictive biomarkers of ICI combination therapy with VEGF inhibitors for HCC
Multiple lines of studies have validated the predictive value of many biomarkers in HCC patients receiving ICI combination therapy with VEGF inhibitors (Table 3). The studies conducted by Zhu et al. [42] and Kuzuya et al. [43] evaluated the on-treatment AFP change in blood of patients. The former study identified that high AFP decrease (≥ 75%) or low AFP increase (≤ 10%) predicted ORR (sensitivity/specificity, 59%/86%; 77%/44%, respectively) and longer median OS (NR vs. 14.2 months, P value < 0.001; 23.7 vs. 10.6 months, P value < 0.001, respectively) and PFS (13.2 vs. 6.7 months, P value < 0.001; 9.9 vs. 5.5 months, P value < 0.001, respectively) than low AFP decrease (< 75%) or high AFP increase (> 10%) in 150 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab); the latter study verified that low AFP ratio (< 1.4) predicted DCR (sensitivity/specificity, 89%/88%) and longer median PFS (30 vs. 6 weeks, P value = 0.0003) than high AFP ratio (≥ 1.4) in 50 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab). The study conducted by Chon et al. [44] measured the pre-treatment PIVKA-II level and NLR and on-treatment change in AFP and PIVKA-II levels and NLR in blood of 121 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab) and confirmed that high AFP decrease (≥ 30%) or PIVKA-II decrease (≥ 50%) or low NLR (< 2.5) predicted higher ORR (43% vs. 22%, P value < 0.05; 50% vs. 26%, P value < 0.05; 39% vs. 19%, P value < 0.05, respectively) than low AFP decrease (< 30%) or PIVKA-II decrease (< 50%) or high NLR (≥ 2.5); high NLR decrease (≥ 10%) predicted better OS than low NLR decrease (< 10%); low PIVKA-II level (< 186 mAU/mL) or NLR (< 2.5) predicted better OS and PFS than high PIVKA-II level (≥ 186 mAU/mL) or NLR (≥ 2.5). In addition, the study conducted by Campani et al. [45] combined the pre-treatment ALBI grade and on-treatment AFP change to stratify 70 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab) and showed that patients with low ALBI grade (grade 1) and high AFP decrease (≥ 20%) had the longest median OS (NR vs. 16.6 vs. 11.8 vs. 5.7 months, P value = 0.046) and PFS (NR vs. 8.6 vs. 5.6 vs. 2.3 months, P value = 0.012), followed by patients with high ALBI grade (grade 2) and high AFP decrease (≥ 20%), patients with low ALBI grade (grade 1) and low AFP decrease (< 20%), and patients with high ALBI grade (grade 2) and low AFP decrease (< 20%). The study conducted by Hatanaka et al. [46] combined the pre-treatment modified albumin-bilirubin (mALBI) grade and AFP level to stratify 426 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab) (255 patients as derivation cohort and 171 patients as validation cohort) and revealed that patients with low mALBI grade (1/2a) and low AFP level (< 100 ng/mL) had the highest OS rate (derivation cohort, 83% vs. 62% vs. 25%, P value < 0.001; validation cohort, 94% vs. 62% vs. 46%, P value < 0.001) and the longest median PFS (derivation cohort, 9.5 vs. 6.6 vs. 3.8 months, P value < 0.001; validation cohort, 9.3 vs. 6.7 vs. 4.7 months, P value = 0.018), followed by patients with high mALBI grade (2b/3) or high AFP level (≥ 100 ng/mL) and patients with high mALBI grade (2b/3) and high AFP level (≥ 100 ng/mL). Moreover, the study conducted by Yang et al. [47] detected the pre-treatment levels of several cytokines in blood of 165 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab) (84 patients as derivation cohort and 81 patients as validation cohort) and found that low interleukin-6 (IL-6) level (< 18.49 pg/mL) predicted higher ORR (derivation cohort, 38% vs. 0%; validation cohort, 29% vs. 7%) and longer OS (derivation cohort, P value = 0.021; validation cohort, P value < 0.001) and PFS (derivation cohort, P value = 0.003; validation cohort, P value = 0.018) than high IL-6 level (≥ 18.49 pg/mL). The study conducted by Giovannini et al. [48] analyzed the pre-treatment percentage of PD-1+ granulocytes in blood of 34 HCC patients treated with PD-L1 ICI (atezolizumab) combined with VEGF inhibitor (bevacizumab) and ascertained that low PD-1+ granulocyte percentage (< 13%) was associated with longer mean time to progression (TTP) (NR vs. 3.2 months, P value < 0.0001) than high PD-1+ granulocyte percentage (≥ 13%). The study conducted by Balcar et al. [49] examined the post-treatment immunoglobulin G (IgG) change in blood of 72 HCC patients treated with PD-1 ICI (such as nivolumab and pembrolizumab) or PD-L1 ICI (atezolizumab) combined with or without VEGF inhibitor (bevacizumab) and demonstrated that low IgG increase (< 14%) was correlated with longer median OS (15.9 vs. 6.4 months, P value = 0.001) and PFS (7.9 vs. 2.9 months, P value = 0.011) than high IgG increase (≥ 14%).
Predictive biomarkers of ICI combination therapy with VEGF inhibitors for HCC
| Biomarkers | Source | Patients and Treatment | Predictive Significancea | Year | References |
|---|---|---|---|---|---|
| On-treatment AFP changeb | Blood | 150 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | High AFP decrease or low AFP increase predicted ORR and longer OS and PFS. | 2022 | Zhu et al. [42] |
| On-treatment AFP changec | Blood | 50 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | Low AFP ratio predicted DCR and longer PFS. | 2022 | Kuzuya et al. [43] |
| Pre-treatment PIVKA-II level or NLR or on-treatment AFP, PIVKA-II, or NLR changed | Blood | 121 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | High AFP or PIVKA-II decrease or low NLR predicted higher ORR. High NLR decrease predicted longer OS. Low PIVKA-II level or NLR predicted longer OS and PFS. | 2023 | Chon et al. [44] |
| Pre-treatment ALBI grade and on-treatment AFP changee | Blood | 70 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | Patients with low ALBI grade and high AFP decrease had the longest OS and PFS, followed by patients with high ALBI grade and AFP decrease, patients with low ALBI grade and AFP decrease, and patients with high ALBI grade and low AFP decrease. | 2023 | Campani et al. [45] |
| Pre-treatment mALBI grade and AFP levelf | Blood | 426 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | Patients with low mALBI grade and AFP level had the highest OS rate and the longest PFS, followed by patients with high mALBI grade or AFP level and patients with high mALBI grade and AFP level. | 2023 | Hatanaka et al. [46] |
| Pre-treatment IL-6 levelg | Blood | 165 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | Low IL-6 level predicted higher ORR and longer OS and PFS. | 2023 | Yang et al. [47] |
| Pre-treatment PD-1+ granulocyte percentageh | Blood | 34 HCC patients treated with PD-L1 ICI combined with VEGF inhibitor | Low PD-1+ granulocyte percentage predicted longer TTP. | 2023 | Giovannini et al. [48] |
| Post-treatment IgG changei | Blood | 72 HCC patients treated with PD-1 or PD-L1 ICI combined with or without VEGF inhibitor | Low IgG increase predicted longer OS and PFS. | 2023 | Balcar et al. [49] |
aOS was defined as the time from treatment initiation to death due to any cause. PFS was defined as the time from treatment initiation to radiological progression or death due to any cause. TTP was defined as the time from treatment initiation to radiological progression (but not death) due to any cause. ORR was defined as the proportion of patients with CR or PR. DCR was defined as the proportion of patients with CR, PR, or SD.
bAFP decrease or increase was defined as the percentage of decrease or increase in serum AFP levels at 4 weeks after treatment initiation relative to pre-treatment levels and was categorized as high (≥ 75%) or low (< 75%) decrease or high (> 10%) or low (≤ 10%) increase.
cAFP ratio was calculated by dividing serum AFP levels at 6 weeks after treatment initiation by pre-treatment levels and was categorized as high (≥ 1.4) or low (< 1.4) ratio.
dPIVKA-II level was categorized as high (≥ 186 mAU/mL) or low (< 186 mAU/mL) level. NLR was calculated by dividing blood neutrophil count by blood lymphocyte count and was categorized as high (≥ 2.5) or low (< 2.5) ratio. AFP, PIVKA-II, or NLR decrease was defined as the percentage of decrease in serum AFP, PIVKA-II, or NLR levels at the first response evaluation after treatment initiation relative to pre-treatment levels and was categorized as high (≥ 30%, ≥ 50%, or ≥ 10) or low (< 30%, < 50%, or < 10) decrease, respectively.
eALBI grade was defined as log10 blood bilirubin level multiplied by 0.66 plus blood albumin level multiplied by -0.085 and was stratified as grade 1 (≤ -2.60), 2 (> -2.60 to ≤ -1.39), or 3 (> -1.39). ALBI grade 2 and 1 were defined as high and low ALBI grade, respectively. AFP decrease was defined as the percentage of decrease in serum AFP levels at 3 weeks after treatment initiation relative to pre-treatment levels and was categorized as high (≥ 20%) or low (< 20%) decrease.
fmALBI grade was calculated by the same formula as ALBI grade and stratified as grade 1 (≤ -2.60), grade 2a (> -2.60 to ≤ -2.27), grade 2b (> -2.27 to ≤ -1.39), or grade 3 (> -1.39). mALBI grade 2b/3 and 1/2a were defined as high and low mALBI grade, respectively. AFP level was categorized as high (≥ 100 ng/mL) or low (< 100 ng/mL) level.
gIL-6 level was categorized as high (≥ 18.49 pg/mL) or low (< 18.49 pg/mL) level.
hPD-1+ granulocyte percentage was defined as the percentage of PD-1-expressing granulocytes on total granulocytes in blood and was categorized as high (≥ 13%) or low (< 13%) percentage.
iIgG increase was defined as the percentage of increase in serum IgG levels at 6 weeks after treatment initiation relative to pre-treatment levels and was categorized as high (≥ 14%) or low (< 14%) decrease.
Abbreviations: ICI, immune checkpoint inhibitor; VEGF, vascular endothelial growth factor; HCC, hepatocellular carcinoma; AFP, alpha-fetoprotein; PD-L1, programmed death ligand 1; ORR, objective response rate; OS, overall survival; PFS, progression-free survival; DCR, disease control rate; PIVKA-II, protein induced by vitamin K absence or antagonist-II; NLR, neutrophil to lymphocyte ratio; ALBI, albumin-bilirubin; mALBI, modified albumin-bilirubin; IL-6, interleukin-6; PD-1, programmed death 1; TTP, time to progression; IgG, immunoglobulin G; CR, complete response; PR, partial response.
Comparative summary of predictive biomarkers of ICI-based mono- and combination therapy for HCC
| Mono- and Combination Therapy | ICIs | ICIs and Other ICIs | ICIs and TKIs | ICIs and VEGF Inhibitors | |
|---|---|---|---|---|---|
| ICI Targets | PD-1 | PD-1 or PD-L1 and CTLA-4 | PD-1 | PD-L1 | |
| Pre-Treatment Biomarkers | Tissue | Tumoral PD-L1 expression level ↑a | Intratumoral CD38+ cell proportion ↑ | ||
| Blood | NLR ↓a PLR ↓ LMR SII ↓ TGF-β level ↓ CRP level ↓ and AFP level ↓ ALBI grade ↓ and age ↑ | NLR ↓ PLR ↓ PNI ↑ | ctDNA TMB ↓ ctDNA MSAF ↓ PD-L1+ CTC count ↓ PIVKA-II level ↓ and metastasis ↓ Nomogram based on ECOG PS, TACE, EHM, Child-Pugh score, ALT, AFP, and PLR ↓ | NLR ↓ IL-6 level ↓ PIVKA-II level ↓ PD-1+ granulocyte percentage ↓ ALBI grade ↓ and AFP decrease ↑b mALBI grade ↓ and AFP level ↓ | |
| Stool | Gut microbiota Erysipelotrichaceae ↑ Veillonellaceae ↓ | Gut microbiota Prevotella 9 ↓ Lachnoclostridium ↑ | |||
| On-Treatment Biomarkers | Blood | NLR ↓ Monocyte index ↑ | AFP decrease ↑ | AFP decrease ↑ | AFP decrease ↑ AFP increase ↓ AFP ratio ↓ NLR decrease ↑ PIVKA-II decrease ↑ |
| Post-Treatment Biomarkers | Blood | NLR ↓ PLR ↓ | AFP decrease ↑ PIVKA-II decrease ↑ | IgG increase ↓ | |
| Predictive Significance | Treatment responses | Higher ORR Higher DCR | Higher ORR Higher DCR | Higher ORR Higher DCR | Higher ORR Higher DCR |
| Treatment outcomes | Longer OS Longer PFS | Longer OS Longer PFS | Longer OS Longer PFS | Longer OS Longer PFS Longer TTP | |
aUpward and downward arrows indicated that high and low levels of biomarkers predicted better treatment responses and outcomes, respectively.
bAlthough classified as a pre-treatment biomarker, this biomarker was based on pre-treatment ALBI grade and on-treatment AFP decrease in prediction.
Abbreviations: ICI, immune checkpoint inhibitor; HCC, hepatocellular carcinoma; TKI, tyrosine kinase inhibitor; VEGF, vascular endothelial growth factor; PD-1, programmed death 1; PD-L1, programmed death ligand 1 NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; LMR, lymphocyte to monocyte ratio; SII, systemic immune-inflammation index; TGF-β, transforming growth factor-beta; CRP, C-reactive protein; AFP, alpha-fetoprotein; ALBI, albumin-bilirubin; PNI, prognostic nutritional index; ctDNA, circulating tumor DNA; TMB, tumor mutation burden; MSAF, maximum somatic allele frequency; CTC, circulating tumor cell; PIVKA-II, protein induced by vitamin K absence or antagonist-II; ECOG PS, Eastern Cooperative Oncology Group performance status; TACE, transarterial chemoembolization; EHM, extrahepatic metastasis; ALT, alanine aminotransferase; IL-6, interleukin-6; mALBI, modified albumin-bilirubin; IgG, immunoglobulin G; ORR, objective response rate; DCR, disease control rate; OS, overall survival; PFS, progression-free survival; TTP, time to progression.
Conclusions
This review comprehensively summarizes the evidence from the literature published so far which validate the predictive significance of a variety of biomarkers at different treatment time points (including pre-treatment, on-treatment, and post-treatment time points) in different sample sources (including tissue, blood, and stool samples) for the treatment responses and outcomes of HCC patients receiving different categories of ICI-based therapies (including ICI mono-therapy and combination therapy with other ICIs or TKIs or VEGF inhibitors) (Table 4). Among the current predictive biomarkers, most are derived from the blood and stool samples of HCC patients, supporting the convenience advantages of the use of noninvasive sampling methods in clinical application. Moreover, the clinical applicability varies among the predictive biomarkers. Certain biomarkers are selective for one category of ICI therapy at one specific treatment time point, such as tumoral PD-L1 expression level, intratumoral CD38+ cell proportion, ctDNA TMB or MSAF, PD-L1+ CTC count, PD-1+ granulocyte percentage, SII, PNI, and IgG change; in contrast, some biomarkers show predictive value for 2 or 3 different categories of therapies at 2 or 3 different treatment time points, such as NLR, PLR, AFP change, and PIVKA-II change. It should be carefully noted that even the same biomarker may have different cut-off values when applied for predicting HCC patients receiving different categories of therapies at different treatment time points. Besides, as a potential way to overcome the inter-patient heterogeneity among HCC patients, several biomarkers combine 2 different factors or even more factors in a nomogram to stratify the patients into more subgroups for prediction, such as CRP level and AFP level, PIVKA-II level and metastasis, ALBI grade and age, ALBI grade and AFP change, and mALBI grade and AFP level. In addition, many predictive biomarkers are based on immune cells or inflammatory cytokines, such as NLR, PLR, LMR, PD-1+ granulocyte percentage, SII, monocyte index, TGF-β, IL-6, and CRP, reflecting the clinical implication of tumor immune microenvironment in the efficacy of ICI therapy for HCC. Additionally, the predictive significance of the composition of gut microbiota, such as Erysipelotrichaceae, Veillonellaceae, Prevotella 9, and Lachnoclostridium, has been validated in HCC patients receiving ICI mono-therapy and combination therapy with TKIs. Considering the impact of gut microbiota-derived metabolites on ICI therapy for cancer [50-52], evaluation of the predictive significance of microbial metabolites in the blood and/or stool samples of HCC patients receiving ICI-based mono- and combination therapies may hold great promise to discover novel predictive biomarkers. Furthermore, non-coding RNAs such as microRNAs and long non-coding RNAs have been closely implicated in cancer and ICI therapy [53, 54]. Whether non-coding RNAs can also serve as predictive biomarkers for ICI therapy in HCC patients is worth further investigation. Last but not the least, since the HCC patient cohorts evaluated in different studies may have different clinicopathological features and receive ICI-based therapies with different drugs (even though sharing the same molecular targets) at different treatment dosages, doses, and dosing intervals, it is quite important to take this issue into consideration when applying the predictive biomarkers to select the most suitable patient for the most suitable treatment for better therapeutic responses and outcomes.
Acknowledgements
Funding
This work was supported by grants from the China Medical University Hospital, Taichung, Taiwan (DMR-112-034).
Author contributions
Chiao-Fang Teng: Conceptualization, funding acquisition, supervision, visualization, writing-original draft, and writing-review and editing. Long-Bin Jeng: Conceptualization and visualization. John Wang: Conceptualization and visualization.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Kulik L, El-Serag HB. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology. 2019;156:477-91 e1
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A. et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-49
3. Cheng KC, Lin WY, Liu CS, Lin CC, Lai HC, Lai SW. Association of different types of liver disease with demographic and clinical factors. Biomedicine (Taipei). 2016;6:16
4. Vaclav T. Surgical treatment of hepatocellular carcinoma. Klin Onkol. 2020;33:30-3
5. Vibert E, Schwartz M, Olthoff KM. Advances in resection and transplantation for hepatocellular carcinoma. J Hepatol. 2020;72:262-76
6. Pillai AA, Ramanathan M, Kulik L. Locoregional Therapies for Hepatocellular Carcinoma: What Has Changed in the Past Ten Years? Clin Liver Dis. 2020;24:681-700
7. Makary MS, Ramsell S, Miller E, Beal EW, Dowell JD. Hepatocellular carcinoma locoregional therapies: Outcomes and future horizons. World J Gastroenterol. 2021;27:7462-79
8. Hou Z, Liu J, Jin Z, Qiu G, Xie Q, Mi S. et al. Use of chemotherapy to treat hepatocellular carcinoma. Biosci Trends. 2022;16:31-45
9. Huang A, Yang XR, Chung WY, Dennison AR, Zhou J. Targeted therapy for hepatocellular carcinoma. Signal Transduct Target Ther. 2020;5:146
10. Liu Z, Liu X, Liang J, Liu Y, Hou X, Zhang M. et al. Immunotherapy for Hepatocellular Carcinoma: Current Status and Future Prospects. Front Immunol. 2021;12:765101
11. Llovet JM, Castet F, Heikenwalder M, Maini MK, Mazzaferro V, Pinato DJ. et al. Immunotherapies for hepatocellular carcinoma. Nat Rev Clin Oncol. 2022;19:151-72
12. Chen L, Flies DB. Molecular mechanisms of T cell co-stimulation and co-inhibition. Nat Rev Immunol. 2013;13:227-42
13. He X, Xu C. Immune checkpoint signaling and cancer immunotherapy. Cell Res. 2020;30:660-9
14. Ramsay AG. Immune checkpoint blockade immunotherapy to activate anti-tumour T-cell immunity. Br J Haematol. 2013;162:313-25
15. Tang S, Ning Q, Yang L, Mo Z, Tang S. Mechanisms of immune escape in the cancer immune cycle. Int Immunopharmacol. 2020;86:106700
16. Bagchi S, Yuan R, Engleman EG. Immune Checkpoint Inhibitors for the Treatment of Cancer: Clinical Impact and Mechanisms of Response and Resistance. Annu Rev Pathol. 2021;16:223-49
17. Naimi A, Mohammed RN, Raji A, Chupradit S, Yumashev AV, Suksatan W. et al. Tumor immunotherapies by immune checkpoint inhibitors (ICIs); the pros and cons. Cell Commun Signal. 2022;20:44
18. Sangro B, Sarobe P, Hervas-Stubbs S, Melero I. Advances in immunotherapy for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18:525-43
19. Pinter M, Jain RK, Duda DG. The Current Landscape of Immune Checkpoint Blockade in Hepatocellular Carcinoma: A Review. JAMA Oncol. 2021;7:113-23
20. Chen Y, Hu H, Yuan X, Fan X, Zhang C. Advances in Immune Checkpoint Inhibitors for Advanced Hepatocellular Carcinoma. Front Immunol. 2022;13:896752
21. Sangro B, Melero I, Wadhawan S, Finn RS, Abou-Alfa GK, Cheng AL. et al. Association of inflammatory biomarkers with clinical outcomes in nivolumab-treated patients with advanced hepatocellular carcinoma. J Hepatol. 2020;73:1460-9
22. Feun LG, Li YY, Wu C, Wangpaichitr M, Jones PD, Richman SP. et al. Phase 2 study of pembrolizumab and circulating biomarkers to predict anticancer response in advanced, unresectable hepatocellular carcinoma. Cancer. 2019;125:3603-14
23. Zhang Y, Lu L, He Z, Xu Z, Xiang Z, Nie RC. et al. C-Reactive Protein Levels Predict Responses to PD-1 Inhibitors in Hepatocellular Carcinoma Patients. Front Immunol. 2022;13:808101
24. Dong D, Zhu X, Wang H, Li L, Wan M, Li S. et al. Prognostic significance of albumin-bilirubin score in patients with unresectable hepatocellular carcinoma undergoing combined immunotherapy and radiotherapy. J Med Imaging Radiat Oncol. 2022;66:662-70
25. Choi WM, Kim JY, Choi J, Lee D, Shim JH, Lim YS. et al. Kinetics of the neutrophil-lymphocyte ratio during PD-1 inhibition as a prognostic factor in advanced hepatocellular carcinoma. Liver Int. 2021;41:2189-99
26. Hung HC, Lee JC, Wang YC, Cheng CH, Wu TH, Lee CF. et al. Response Prediction in Immune Checkpoint Inhibitor Immunotherapy for Advanced Hepatocellular Carcinoma. Cancers (Basel). 2021;13:1607
27. Dharmapuri S, Ozbek U, Lin JY, Sung M, Schwartz M, Branch AD. et al. Predictive value of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in advanced hepatocellular carcinoma patients treated with anti-PD-1 therapy. Cancer Med. 2020;9:4962-70
28. Huang R, Zheng Y, Zou W, Liu C, Liu J, Yue J. Blood Biomarkers Predict Survival Outcomes in Patients with Hepatitis B Virus-Induced Hepatocellular Carcinoma Treated with PD-1 Inhibitors. J Immunol Res. 2022;2022:3781109
29. Jeon SH, Lee YJ, Kim HD, Nam H, Ryoo BY, Park SH. et al. Dynamic changes in peripheral blood monocytes early after anti-PD-1 therapy predict clinical outcomes in hepatocellular carcinoma. Cancer Immunol Immunother. 2023;72:371-84
30. Mao J, Wang D, Long J, Yang X, Lin J, Song Y. et al. Gut microbiome is associated with the clinical response to anti-PD-1 based immunotherapy in hepatobiliary cancers. J Immunother Cancer. 2021;9:e003334
31. Ng HHM, Lee RY, Goh S, Tay ISY, Lim X, Lee B. et al. Immunohistochemical scoring of CD38 in the tumor microenvironment predicts responsiveness to anti-PD-1/PD-L1 immunotherapy in hepatocellular carcinoma. J Immunother Cancer. 2020;8:e000987
32. Muhammed A, Fulgenzi CAM, Dharmapuri S, Pinter M, Balcar L, Scheiner B. et al. The Systemic Inflammatory Response Identifies Patients with Adverse Clinical Outcome from Immunotherapy in Hepatocellular Carcinoma. Cancers (Basel). 2021;14:186
33. Shao YY, Liu TH, Hsu C, Lu LC, Shen YC, Lin ZZ. et al. Early alpha-foetoprotein response associated with treatment efficacy of immune checkpoint inhibitors for advanced hepatocellular carcinoma. Liver Int. 2019;39:2184-9
34. Lee PC, Chao Y, Chen MH, Lan KH, Lee CJ, Lee IC. et al. Predictors of Response and Survival in Immune Checkpoint Inhibitor-Treated Unresectable Hepatocellular Carcinoma. Cancers (Basel). 2020;12:182
35. Hsu WF, Wang HW, Chen CK, Lai HC, Chuang PH, Tsai MH. et al. Alpha-fetoprotein response predicts treatment outcomes in patients with unresectable hepatocellular carcinoma receiving immune checkpoint inhibitors with or without tyrosine kinase inhibitors or locoregional therapies. Am J Cancer Res. 2021;11:6173-87
36. Sun X, Mei J, Lin W, Yang Z, Peng W, Chen J. et al. Reductions in AFP and PIVKA-II can predict the efficiency of anti-PD-1 immunotherapy in HCC patients. BMC Cancer. 2021;21:775
37. Li X, Sun W, Ding X, Li W, Chen J. Prognostic model of immune checkpoint inhibitors combined with anti-angiogenic agents in unresectable hepatocellular carcinoma. Front Immunol. 2022;13:1060051
38. Guo DZ, Zhang SY, Dong SY, Yan JY, Wang YP, Cao Y. et al. Prognostic model for predicting outcome and guiding treatment decision for unresectable hepatocellular carcinoma treated with lenvatinib monotherapy or lenvatinib plus immunotherapy. Front Immunol. 2023;14:1141199
39. Xu G, Cui L, Li J, Wang Q, Li P, Xia X. et al. bMSAF is a prognostic predictor for advanced hepatocellular carcinoma patients treated with immune checkpoint inhibitor camrelizumab and anti-angiogenic agent apatinib combination therapy. Clin Transl Med. 2022;12:e1086
40. Su K, Guo L, He K, Rao M, Zhang J, Yang X. et al. PD-L1 expression on circulating tumor cells can be a predictive biomarker to PD-1 inhibitors combined with radiotherapy and antiangiogenic therapy in advanced hepatocellular carcinoma. Front Oncol. 2022;12:873830
41. Lee PC, Wu CJ, Hung YW, Lee CJ, Chi CT, Lee IC. et al. Gut microbiota and metabolites associate with outcomes of immune checkpoint inhibitor-treated unresectable hepatocellular carcinoma. J Immunother Cancer. 2022;10:e004779
42. Zhu AX, Dayyani F, Yen CJ, Ren Z, Bai Y, Meng Z. et al. Alpha-Fetoprotein as a Potential Surrogate Biomarker for Atezolizumab + Bevacizumab Treatment of Hepatocellular Carcinoma. Clin Cancer Res. 2022;28:3537-45
43. Kuzuya T, Kawabe N, Hashimoto S, Miyahara R, Sawaki A, Nakano T. et al. Early Changes in Alpha-Fetoprotein Are a Useful Predictor of Efficacy of Atezolizumab plus Bevacizumab Treatment in Patients with Advanced Hepatocellular Carcinoma. Oncology. 2022;100:12-21
44. Chon YE, Cheon J, Kim H, Kang B, Ha Y, Kim DY. et al. Predictive biomarkers of survival in patients with advanced hepatocellular carcinoma receiving atezolizumab plus bevacizumab treatment. Cancer Med. 2023;12:2731-8
45. Campani C, Bamba-Funck J, Campion B, Sidali S, Blaise L, Ganne-Carrie N. et al. Baseline ALBI score and early variation of serum AFP predicts outcomes in patients with HCC treated by atezolizumab-bevacizumab. Liver Int. 2023;43:708-17
46. Hatanaka T, Kakizaki S, Hiraoka A, Tada T, Hirooka M, Kariyama K. et al. Development and validation of a modified albumin-bilirubin grade and alpha-fetoprotein score (mALF score) for hepatocellular carcinoma patients receiving atezolizumab and bevacizumab. Hepatol Int. 2023;17:86-96
47. Yang H, Kang B, Ha Y, Lee SH, Kim I, Kim H. et al. High serum IL-6 correlates with reduced clinical benefit of atezolizumab and bevacizumab in unresectable hepatocellular carcinoma. JHEP Rep. 2023;5:100672
48. Giovannini C, Suzzi F, Tovoli F, Bruccoleri M, Marseglia M, Alimenti E. et al. Low-Baseline PD1+ Granulocytes Predict Responses to Atezolizumab-Bevacizumab in Hepatocellular Carcinoma. Cancers (Basel). 2023;15:1661
49. Balcar L, Bauer D, Pomej K, Meischl T, Mandorfer M, Reiberger T. et al. Early changes in immunoglobulin G levels during immune checkpoint inhibitor treatment are associated with survival in hepatocellular carcinoma patients. PLoS One. 2023;18:e0282680
50. Hayase E, Jenq RR. Role of the intestinal microbiome and microbial-derived metabolites in immune checkpoint blockade immunotherapy of cancer. Genome Med. 2021;13:107
51. Zhao H, Wang D, Zhang Z, Xian J, Bai X. Effect of Gut Microbiota-Derived Metabolites on Immune Checkpoint Inhibitor Therapy: Enemy or Friend? Molecules. 2022;27:4799
52. Luu M, Schutz B, Lauth M, Visekruna A. The Impact of Gut Microbiota-Derived Metabolites on the Tumor Immune Microenvironment. Cancers (Basel). 2023;15:1588
53. Smolle MA, Prinz F, Calin GA, Pichler M. Current concepts of non-coding RNA regulation of immune checkpoints in cancer. Mol Aspects Med. 2019;70:117-26
54. Shek D, Read SA, Akhuba L, Qiao L, Gao B, Nagrial A. et al. Non-coding RNA and immune-checkpoint inhibitors: friends or foes? Immunotherapy. 2020;12:513-29
Author contact
![]() Corresponding author: Chiao-Fang Teng, Graduate Institute of Biomedical Sciences, China Medical University, No. 91, Hsueh-Shih Rd., Northern Dist., Taichung 404, Taiwan. E-mail: chiaofangtengcom.
Corresponding author: Chiao-Fang Teng, Graduate Institute of Biomedical Sciences, China Medical University, No. 91, Hsueh-Shih Rd., Northern Dist., Taichung 404, Taiwan. E-mail: chiaofangtengcom.

 Global reach, higher impact
Global reach, higher impact