3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(6):1750-1761. doi:10.7150/jca.91089 This issue Cite
Research Paper
Dual Inhibition of B7-H3 and EGFR Overcomes Acquired Chemoresistance in Colon Adenocarcinoma
1. Department of Pathology, China Medical University Hospital, China Medical University, Taichung 40402, Taiwan.
2. Proton Therapy and Science Center, China Medical University Hospital, China Medical University, Taichung 40402, Taiwan.
3. Lab of Precision Medicine, Feng-Yuan Hospital, Ministry of Health and Welfare, Taichung 42055, Taiwan.
4. Department of Pathology, Asia University Hospital, Asia University, Taichung 41354, Taiwan.
5. Department of Colorectal Surgery, China Medical University HsinChu Hospital, China Medical University, HsinChu 302, Taiwan.
6. Department of Colorectal Surgery, China Medical University Hospital, China Medical University, Taichung 40402, Taiwan.
7. Department of Surgery, School of Medicine, China Medical University, Taichung 40402, Taiwan.
8. School of Chinese Medicine, China Medical University, Taichung 40402, Taiwan.
9. Department of Radiation Oncology, China Medical University Hospital, China Medical University, Taichung, Taiwan.
10. Department of Radiotherapy, School of Medicine, China Medical University, Taichung 40402, Taiwan.
11. Department of Biomedical Imaging and Radiological Science, China Medical University, Taichung 40402, Taiwan.
12. Translation Research Core, China Medical University Hospital, China Medical University, Taichung 40402, Taiwan.
13. Cancer Biology and Precision Therapeutics Center, China Medical University, Taichung 40402, Taiwan.
* These authors have contributed equally to this work and share first authorship.
Abstract
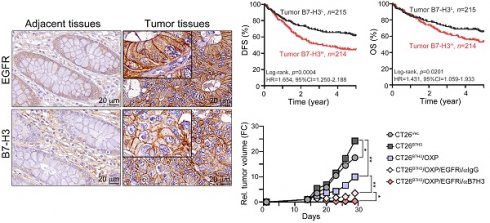
Despite advances in therapeutic strategies for colorectal cancer (CRC), CRC has a high disease incidence with significant morbidity and mortality worldwide. Notably, immunotherapy has shown limited efficacy in treating metastatic CRC, underscoring the need for alternative immunotherapeutic targets for the management of metastatic colorectal cancer (mCRC). In the present study, we evaluated the levels of the immune checkpoint proteins PD-L1, PD-L2 and B7-H3 in a large cohort retrospective study. We found that tumor B7-H3 (52.7%) was highly expressed in primary tumors compared to that in PD-L1 (33.6%) or PD-L2 (34.0%). Elevated B7-H3 expression was associated with advanced stage and the risk of distant metastasis and correlated with poor disease-free survival (DFS), suggesting that tumor B7-H3 was an independent prognostic factor associated with worse DFS in colon adenocarcinoma patients (COAD), especially high-risk COAD patients who received adjuvant chemotherapy. Furthermore, we found that B7-H3 significantly promoted cell proliferation and tumor growth in CRC. B7-H3 may stabilize EGFR to activate its downstream pathway for cancer cell proliferation and resistance to oxaliplatin (OXP). Dual targeting of B7-H3 and EGFR markedly rescued the susceptibility to chemotherapy in colorectal cancer cells in vitro and in vivo. Overall, these results showed that B7-H3 exhibited a high prevalence in COAD patients and was significantly associated with worse prognosis in COAD patients. Dual targeting of B7-H3 and EGFR signaling might be a potential therapeutic strategy for high-risk COAD patients.
Keywords: Colorectal cancer, B7-H3, Intratumoral infiltrating lymphocytes, PD-L1

 Global reach, higher impact
Global reach, higher impact