3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2021; 12(9):2624-2632. doi:10.7150/jca.53215 This issue Cite
Research Paper
Region-specific Risk Factors for Pelvic Lymph Node Metastasis in Patients with Stage IB1 Cervical Cancer
1. Department of Obstetrics and Gynecology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China.
2. Department of Pathology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China.
3. University Clinic for Medical Radiation Physics, Medical Campus Pius-Hospital, Carl von Ossietzky University Oldenburg, Germany.
* Jing Zhao and Jing Cai contributed equally to this work.
Abstract
Objectives: We aimed to identify the risk factors associated with pelvic lymph node metastasis (LNM) at each anatomic location in patients with stage IB1 cervical cancer.
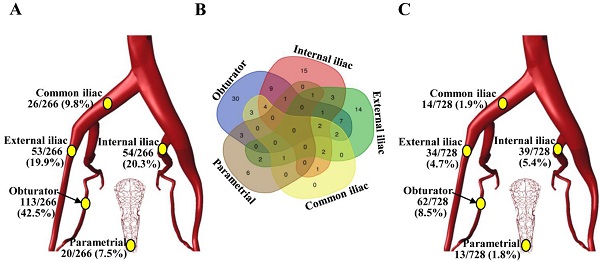
Methods: A primary cohort of 728 patients with stage IB1 cervical cancer who underwent radical hysterectomy and systematic pelvic lymphadenectomy were retrospectively studied. All removed pelvic nodes (N=20,134) were pathologically examined. The risk factors for LNM in different anatomic regions (obturator, internal iliac, external iliac, and common iliac) were evaluated by multivariate logistic regression analyses. Nomograms were generated from the primary cohort and validated in another external cohort (N=242). The performance of the nomogram was assessed by its calibration and discrimination. Overall survival and progression-free survival in patients with different LNM patterns were compared.
Results: LNM was found in 266 (1.3%) removed nodes and 106 (14.6%) patients. The incidences of LNM at the obturator, internal iliac, external iliac, common iliac, and parametrial regions were 8.5%, 5.4%, 4.7%, 1.9% and 1.8%, respectively. Among others, tumour size and lymph-vascular space invasion (LVSI), which are preoperatively assessable, were identified as independent risk factors of LNM in the common iliac region and the lower pelvis, respectively, and age was an additional independent risk factor of obturator LNM. The negative predictive values of tumour size <2 cm for common iliac LNM and negative LVSI combined with older age (> 50 years) for obturator LNM were 100% and 98.7%, respectively. A nomogram of these two factors showed good calibration and discrimination (concordance index, 0.761 in the primary cohort and 0.830 in validation cohort). The patients with common iliac LNM had poorer survival than those with LNM confined to the lower pelvis, while the differences in survival between patients with LNM confined to one node, one region or single side and those with more widely spreading LNM were not statistically significant.
Conclusions: Tumour size, LVSI and age are region-specific risk factors for pelvic LNM in IB1 cervical cancer, which could be used to allocate the appropriate extent of pelvic lymphadenectomy.
Keywords: cervical cancer, lymph node metastasis, lymphadenectomy, early stage.

 Global reach, higher impact
Global reach, higher impact