Impact Factor
ISSN: 1837-9664
J Cancer 2025; 16(6):1860-1872. doi:10.7150/jca.109589 This issue Cite
Research Paper
Multi-Omics Profiling Identifies a High-Risk Subgroup of Breast Cancer Stem Cells for Prognostic Stratification and Personalized Treatment
1. The First Department of Breast Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin's Clinical Research Center for Cancer, National Clinical Research Center for Cancer, Key Laboratory of Breast Cancer Prevention and Therapy, Tianjin Medical University Cancer Institute and Hospital, Tianjin Medical University, Tianjin, 300060, China.
2. Department of Thoracic Oncology, Tianjin Lung Cancer Center, Key Laboratory of Cancer Prevention and Therapy, Tianjin's Clinical Research Center for Cancer, Tianjin Medical University Cancer Institute and Hospital, Tianjin Medical University, Tianjin, 300060, China.
3. Department of General Surgery, Tianjin Medical University General Hospital, Tianjin Key Laboratory of Precise Vascular Reconstruction and Organ Function Repair, Tianjin General Surgery Institute, Tianjin, 300052, China.
4. Tianjin Medical University, Tianjin, 300070, China.
5. Immunology Department, Key Laboratory of Immune Microenvironment and Disease (Ministry of Education), Tianjin Medical University, Tianjin, 300070, China.
# These authors contributed equally to this work.
Received 2024-12-29; Accepted 2025-2-16; Published 2025-2-28
Abstract
Background: Breast cancer is the most prevalent malignancy among females worldwide. Extensive research has highlighted cancer stem cells (CSCs) as critical drivers of tumor initiation, progression, recurrence, and therapy resistance. However, the heterogeneity of breast cancer stem cells (BCSCs) and their dynamic roles within the tumor microenvironment remain inadequately understood.
Methods: This study utilized the single-cell RNA sequencing dataset to categorize BCSCs into two subgroups within the breast cancer microenvironment and investigate their pseudo-time developmental dynamics. Bulk transcriptomic data from TCGA-BRCA were integrated to assess the prognostic significance and infiltration abundance of the BCSCs-2 subgroup. Functional enrichment, co-expression network analysis, and somatic mutation profiling were performed to elucidate key biological pathways and genetic features. Additionally, drug sensitivity analyses were conducted using the Connectivity Map database to identify potential therapeutic strategies.
Results: A total of 459 BCSCs were identified and further classified into two distinct subpopulations: BCSCs-1 and BCSCs-2. High infiltration of BCSCs-2 was associated with poor prognosis and an immunosuppressive tumor microenvironment. Co-expression network analysis identified 16 key genes linked to BCSCs-2, while somatic mutation analysis revealed distinct mutation patterns associated with its infiltration. Drug sensitivity analysis suggested that patients with high BCSCs-2 infiltration could benefit from classical chemotherapy agents, such as Cisplatin, and other novel therapeutic compounds.
Conclusions: This study offers novel insights into the heterogeneity and functional roles of BCSCs in breast cancer. The findings highlight the prognostic and therapeutic importance of the BCSCs-2 subgroup, providing potential biomarkers and therapeutic targets for precision medicine in breast cancer management.
Keywords: breast cancer, cancer stem cells, heterogeneity, multi-omics, tumor microenvironment
Introduction
With the advancement of medical technology and the increase in human life expectancy, cancer has emerged as a significant global public health concern[1, 2]. Notably, breast cancer poses a particularly severe threat to female health worldwide, accounting for one-quarter of all newly diagnosed cancer cases and one-sixth of cancer-related deaths among females globally[3]. Although breast cancer mortality rates have declined in some countries, its incidence continues to rise, increasing by 1% annually from 2012 to 2021[4]. Molecular subtyping of breast cancer has become a widely accepted approach for guiding therapy in breast cancer patients[5]. However, accumulating evidence indicates that molecular subtyping cannot completely capture the heterogeneity of breast cancer. Therefore, it is urgent to deeply explore the tumor microenvironment to address this challenge.
Cancer stem cells (CSCs) are a subset of tumor cells that exhibit stem cell-like characteristics and have been recognized as key players in the initiation and progression of tumors[6]. These cells form a rare and highly organized hierarchical structure within the tumor and are considered the root cause of cancer recurrence and resistance to treatment. As such, CSCs have been a central focus of cancer research[7]. Cancer stem cells possess traits such as tumor initiation, self-renewal, multipotency, plasticity, and cancer stemness as a cellular state. These characteristics not only contribute to tumor progression and dissemination but also indicate that CSCs are in a dynamic and variable state within the tumor microenvironment[7]. Clinically, treatments targeting cancer stem cells have been tested in some blood cancers and solid tumors[6]. In lung cancer, Notch activity has been shown to identify cancer stem-like populations, and its inhibition may serve as a potential target for treating lung adenocarcinoma[8]. In summary, increasing evidence suggests that many cancers are driven by CSCs, which possess self-renewal and unlimited differentiation potential. Therefore, research on CSCs is crucial for the development of more effective cancer therapies.
Breast cancer stem cells (BCSCs) were first identified in 2003 using a model in which human breast cancer cells grew in immunodeficient mice[9, 10]. With deeper investigation into BCSCs, it has been found that they are divided into several distinct subpopulations, each with different functions[11, 12]. At the same time, potential therapeutic strategies targeting BCSCs have been reported. For example, treatment with bevacizumab, combined with the dual-topoisomerase inhibitor TOPO-1 and the HIF-1α inhibitor camptothecin, has shown potential for effectively targeting CSCs under hypoxic conditions[13]. Additionally, some reports indicate that CSC-targeting drugs can significantly enhance the effectiveness of anti-angiogenic therapies by targeting key pathways involved in tumor growth and vascularization[14]. Meanwhile, the plasticity of BCSCs has attracted significant research attention[15]. This suggests that BCSCs may play a key role in breast cancer treatment and hold substantial clinical translational value. However, our understanding of BCSCs is still in its early stages. Given the dynamic nature of BCSCs within the tumor microenvironment, it is essential to identify their subpopulations.
Although previous studies have suggested that targeting CSCs may enhance the efficacy of traditional cancer treatments, the identification and eradication of CSCs remain challenging[16]. With the development and maturation of single-cell sequencing technology, we are now able to more reliably identify CSCs within the tumor microenvironment[17, 18]. Therefore, this study aims to utilize single-cell RNA sequencing to identify CSCs in breast cancer and classify them into different subpopulations. We explored the developmental trajectory of different BCSCs and their association with patient prognosis. Furthermore, we investigated the roles and functions of these subpopulations within the tumor microenvironment. We also identified key cellular markers and co-mutation patterns of the newly discovered BCSCs. Notably, drug sensitivity analysis further highlighted the clinical translational value of our research. Overall, this study provides a new perspective for understanding breast cancer from the viewpoint of CSCs and offers a novel potential therapeutic strategy for breast cancer treatment.
Materials and Methods
Data Acquisition and Pre-processing
Bulk-RNA transcriptome data, single nucleotide variant (SNV) data, and survival time-to-event data of corresponding patients were obtained from the BRCA cohort in The Cancer Genome Atlas (TCGA). The 'TCGAbiolinks' package (v2.26.0) was used to obtain the above data. Patients were included based on following criteria: 1. Complete expression profiles and follow-up information; 2. Diagnosed with primary breast cancer. In summary, a total of 1080 breast cancer patients with bulk RNA data were enrolled in study. The single-cell RNA sequencing dataset (GSE180286, https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE180286) was obtained from the Gene Expression Omnibus (GEO) Series. Of note, 5 single-cell profiles of primary sites were included for subsequent analyses.
The Seurat (v4.3.0) package was used for quality control and dimensionality reduction of scRNA-seq profiles. Routine quality control (QC) was performed using the following threshold criteria: genes detected per cell ≥ 200; nCount of RNA ≥ 200; proportion of reads mapped to mitochondrial genes ≤ 20%; proportion of reads mapped to hemoglobin genes ≤ 1%; and log10FeaturePerUMI ≥ 0.8. Potential doublets and batch effects were removed using the DoubletFinder package (v2.0.3)[19] and Harmony (v1.2.0)[20], respectively. The number of low-quality cells removed for each sample to 0.8% of the total cell count. SCTransform (v0.3.5)[21] was conducted for normalization, variance stabilization, and scaling of scRNA-seq data. Cell population annotation was performed based on biological markers obtained from online database[22].
Downstream Analysis of scRNA-seq Data
The SCP (v0.4.7.9) package was used to conduct pseudo-time analysis to simulate the developmental trajectory of cells and identify key markers, functional annotations, and pathway analysis among different cell clusters. Specifically, the Slingshot tool was used to calculate the similarity and distance between cells, thereby inferring the dynamic trajectories of cells in a specific biological process within a low-dimensional space. The single-cell matrix and bulk transcriptome data were integrated using CIBERSORTx (https://cibersortx.stanford.edu/)[23] to estimate the infiltration abundance of BCSCs-2 in different samples. The single-cell gene matrix of BCSCs was used as the reference, while the bulk RNA matrix was utilized for inference. The parameters for the single-cell input options were set as follows: 1. min.Expression = 0.75; 2. Replicates = 5; 3. Sampling = 0.5. Additionally, the absolute mode was selected to infer the abundance of cell clusters in the sample tissues. Subsequently, the survival outcomes of different groups based on the best cut-off value was evaluated using the survminer (v0.4.9) R package through Kaplan-Meier analysis.
Enrichment Analysis
Differential gene expression analysis was performed using the limma (v3.54.2) package. Differentially expressed genes were identified based on the P-value, with P < 0.05 considered significant. All differential genes were reordered by the value of fold change. Subsequently, gene set enrichment analysis (GSEA) provided by the clusterProfiler (v4.12.2) R package[24] was used to further identify potential functional pathways associated with BCSCs-2, and the GseaVis (v0.0.5) package was used for visualization.
Co-expression Network Analysis
The "hdwgcna" (v0.2.18) R package was used to analyze co-expressed gene modules in breast cancer-associated stem cells. Weighted Gene Co-expression Network Analysis (WGCNA) is a commonly used method for gene expression data analysis that identifies gene modules and investigates the association between these modules and external sample characteristics. Specifically, based on the expression profile variation of BCSCs, we chose 12 as the soft threshold and divided them into 13 different modules. The FindMarkers function in the Seurat package was used to identify the top genes of the BCSC-2 cell population, and the ggvenn (v0.1.10) package was used to perform an intersection and obtain the list of genes of interest.
Somatic Mutation Landscape Analysis
The TCGAbiolinks package (v2.26.0) was used to access the required somatic mutation data from the TCGA database. The landscape of masked somatic mutation profiles between different BCSCs-2 infiltration abundances was analyzed using the maftools (v2.20.0) package[25]. The significance of gene pairs between different groups was identified using Fisher's exact test. Additionally, a heatmap was generated to illustrate the co-occurrence and mutual exclusivity of mutations across genes.
Drug Sensitivity Analysis
Connectivity Map (CMap, https://clue.io/)[26] was used to further explore potential corresponding drugs by comparing gene expression profiles. CMap is a reliable bioinformatics database and tool that can identify candidate compounds capable of reversing specific disease-associated gene expression patterns, thereby providing insights for novel drug development. The ggplot2 (v3.5.1) package and ComplexHeatmap (v2.16.0) package were used for the visualization of CMap results.
In addition, the oncoPredict (v1.2) package was used to analyze the drug sensitivity of several chemotherapeutics between distinct groups.
Statistics
All statistical methods were performed using R software (version 4.2.2). Specific statistical details can be found in the corresponding material and methods section.
Results
Identification of Breast Cancer Stem Cells
As illustrated in Figure 1, this study aims to investigate the presence of breast cancer stem cells in the breast cancer microenvironment and explore their potential biological functions. After the standardized quality control process of the single-cell RNA transcript profile, potential low-quality doublets were removed to ensure the reliability of the data used for subsequent analysis.
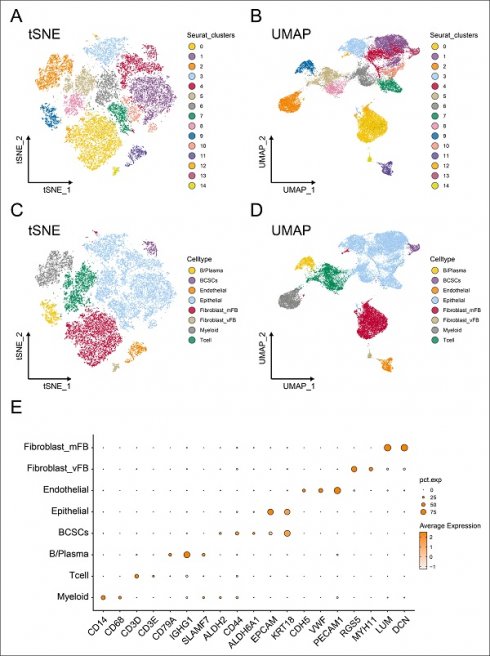
Tracking and annotating breast cancer stem cells from single-cell transcriptome data. (A-B) Reduced dimension maps of t-Distributed Neighbor Embedding (t-SNE) and the Uniform Manifold Approximation and Projection (UMAP) based on clusters. (C-D) Reduced dimension maps of t-Distributed Neighbor Embedding (t-SNE) and the Uniform Manifold Approximation and Projection (UMAP) based on cell types. (E) The expression levels of cell marker genes in different cell population annotations were represented by dot plots.
Subsequently, we applied t-Distributed Neighbor Embedding (t-SNE) (Figure 1A) and Uniform Manifold Approximation and Projection (UMAP) (Figure 1B) methods for dimensionality reduction, resulting in the partitioning of the 25,665 cells into 14 distinct clusters with the resolution set as 0.5. Furthermore, based on previously reported biologically specific markers of different cell populations, we constructed the single-cell profile and identified 459 breast cancer stem cells (BCSCs), 949 B cells/plasma cells, 792 endothelial cells, 12173 epithelial cells, 2385 myeloid cells, 3074 T cells, 5632 myofibroblasts, and 201 vascular fibroblasts (Figure 1C-D).
It is worth noting that CD14 and CD68 were used to label myeloid cells, while CD3D and CD3E served as markers for T cells. CD79A, IGHG1, and SLAMF7 were utilized to identify B cells and plasma cells. EPCAM and KRT18 were employed to label epithelial cells, whereas ALDH2, CD55, and ALDH6A1 were used to identify breast cancer stem cells. CDH5, VWF, and PECAM1 were markers for endothelial cells, and RGS5, MYH11, LUM, and DCN were used to label fibroblasts (Figure 1E).
Cell Trajectory of Breast Cancer Stem Cells
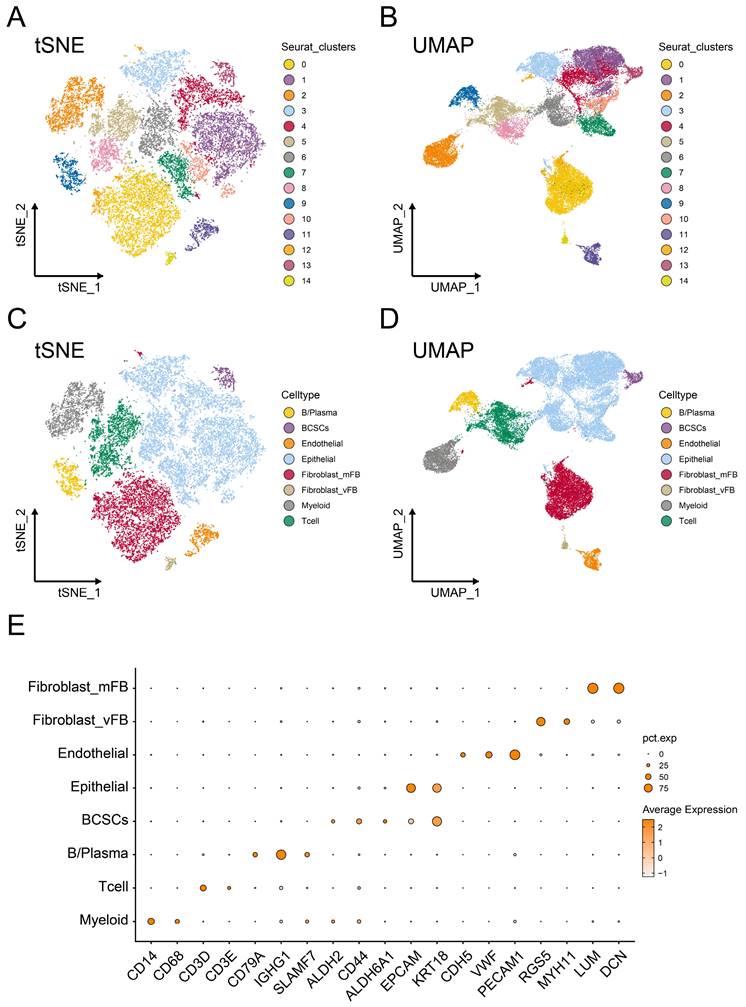
Cells in the tumor microenvironment are constantly undergoing dynamic changes. Therefore, to further explore the heterogeneity of breast cancer stem cells in the tumor microenvironment, we conducted pseudo-time analysis. Two distinct subgroups and a potential lineage evolution of breast cancer stem cells were identified. BCSCs showed a tendency to develop from BCSCs-1 to BCSCs-2 (Figure 2A). The top 5 markers of each cell subgroup were illustrated in supplementary Figure S1A. In order to further study the potential biological functions of BCSCs, the changes in gene expression between different cell populations and pseudo-time stages were examined. The functional context of the biological processes associated with these genes was also investigated through Gene Ontology Biological Process (GO_BP) terms (Figure 2B).
Notably, during the developmental trajectory of cells, breast cancer stem cells (BCSCs) tend to express genes such as IER3 and GADD45B at the early stage, while genes like NNMT and LDHB are preferentially expressed in the BCSCs-2 developmental state. In terms of their biological functions, early-stage BCSCs-1 cells could regulate stress responses and signal transduction by inhibiting protein kinase activity through pathways like 'Negative regulation of protein kinase activity' and 'Negative regulation of protein phosphorylation'. The enrichment of BCSCs-2 cells in the 'Pyridine nucleotide metabolic process' and 'NAD biosynthetic process' suggested a metabolically active phenotype. These results suggest that the intrinsic lineage evolution of BCSCs may be accompanied by the evolution of distinct biological functions.
Tumor Prognostic Value and Potential Biological Role of BCSCs-2 Cells
In order to reveal the clinical significance of breast cancer stem cells, we used the sc-RNA matrix to estimate the abundance of stem cell infiltration levels of patients in the TCGA-BRCA cohort. The high- and low- infiltration groups were determined by the best cut-off value based on the absolute score of each cluster. Interestingly, a high abundance level of BCSCs-1was found to have no significant prognostic value (Figure 2C), while a high abundance level of BCSCs-2 was associated with poor prognosis (p < 0.05, Figure 2D). Based on these findings, we investigated whether BCSCs-2 might influence prognosis through specific biological functions.
The transcriptome data were used to obtain the list of differentially expressed genes, which were sorted by fold change and analyzed by GSEA functional enrichment. We observed a downregulation of the following pathways in the high BCSCs-2 group: 'Epithelial Mesenchymal Transition' (NES: 2.09, Adjusted p-value: < 0.001, Figure 3A), 'PD-1 Signaling' (NES: 2.67, Adjusted p-value: < 0.001, Figure 3B), 'Signaling By Interleukins' (NES: 2.03, Adjusted p-value: < 0.001, Figure 3C), 'Interleukin 2 Signaling' (NES: 2.00, Adjusted p-value: < 0.001, Figure 3D, Supplementary Table S1), 'IL-6 JAK/STAT3 Signaling' (NES: 2.26, Adjusted p-value: < 0.001, Figure 3E), and 'Interleukin 10 Signaling' (NES: 2.44, Adjusted p-value: < 0.001, Figure 3F). These findings indicate that the high infiltration level of BCSCs-2 may be associated with heightened tumor malignancy, enhanced tumor stemness, and the formation of an immunosuppressive microenvironment.
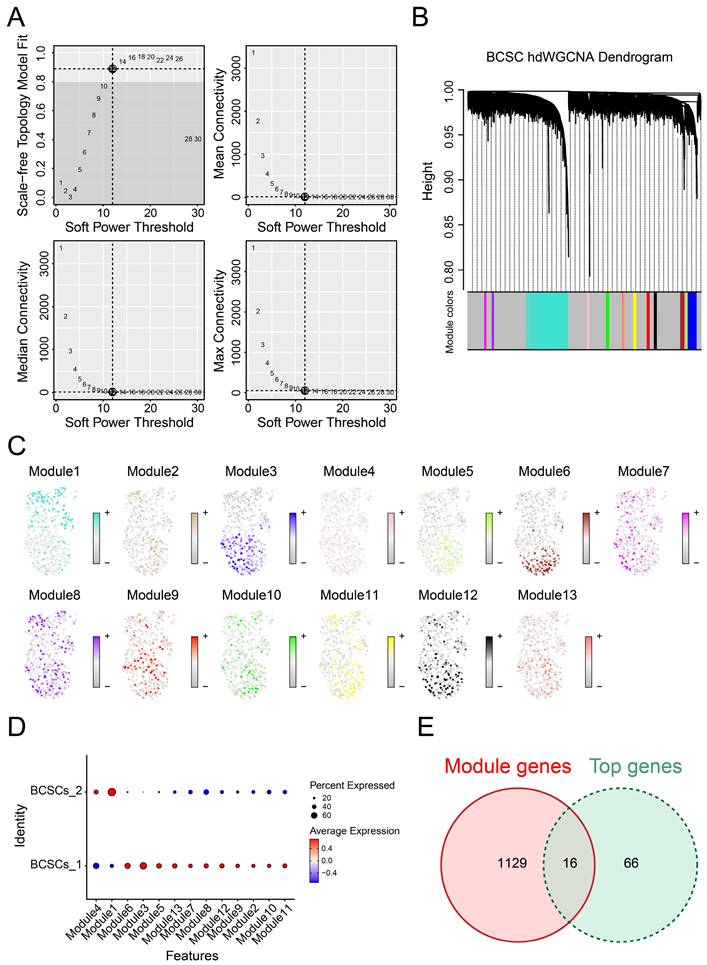
Identification of Gene Co-expression Modules Among BCSCs
Due to the correlation between breast cancer stem cell subpopulations and prognosis as well as biological functions, it is essential to explore the co-expression gene networks that play significant roles in these two subgroups. To achieve optimal connectivity, we constructed a scale-free network for BCSCs and set the soft threshold to 12 (Figure 4A-B). Finally, we identified a total of 13 modules and found that the genes in module 1 were most enriched and played a critical role in BCSCs-2, while they were scarcely enriched in BCSCs-1(Figure 4C-D), suggesting these genes could be important co-expressed genes. In addition, we performed differential gene analysis between BCSCs-2 and other types of cells to obtain the top marker genes of BCSCs-2. By integrating the above gene lists, we identified 16 intersecting genes (Figure 4E), including KMT2E, IFITM3, MAGED2, TM4FSF1, GSTP1, SRI, CD59, SLC39A6, LIMCH1, ATP1B1, DSP, SYNE2, RARRES3, TMC5, SLC40A1, and TM4SF18. In summary, the above genes may serve as potential diagnostic markers and core genes of BCSCs-2.
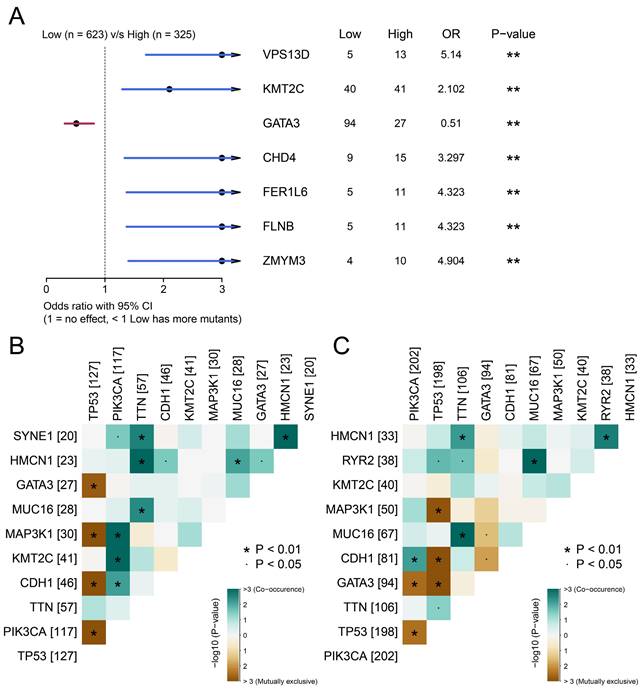
BCSCs-2 Cells Possessed More Somatic Co-mutations
The above results confirmed the prognostic value of BCSCs-2, and we next explored the factors that may relate to the infiltration level of BCSCs. After integrating SNV data and removing invalid entries, we further analyzed the significant differences in somatic mutations between the two groups using Fisher's exact test. Genes such as VPS13D (p < 0.01), KMT2C (p < 0.01), CHD4 (p < 0.01), FER1L6 (p < 0.01), FLNB (p < 0.01), and ZMYM4 (p < 0.01) possessed more mutation frequencies in the high BCSCs-2 infiltration group. Meanwhile, GATA3 (p < 0.01) was found to possess more mutations in the low infiltration group (Figure 5A).
Co-mutation patterns were more abundant in the high BCSCs-2 infiltration abundance group than in the other group (Figure 5B-5C). These findings indicated significant differences in the somatic mutation spectrum between the two groups and revealed a subtle link between somatic variation and BCSCs-2.
Developmental trajectory and prognostic analysis of BCSCs. (A) Pseudo-time developmental trajectories of BCSCs. BCSCs tended to develop from BCSCs-1 to BCSCs-2. (B) Changes in gene expression of BCSCs in Lineage 1, with functional enrichment results of GO_BP for different gene lists shown on the right. (C) Kaplan-Meier curves describing overall survival (OS) in breast cancer patients with different infiltration levels of BCSC-1. (D) Kaplan-Meier curves describing overall survival (OS) in breast cancer patients with different infiltration levels of BCSC-2.
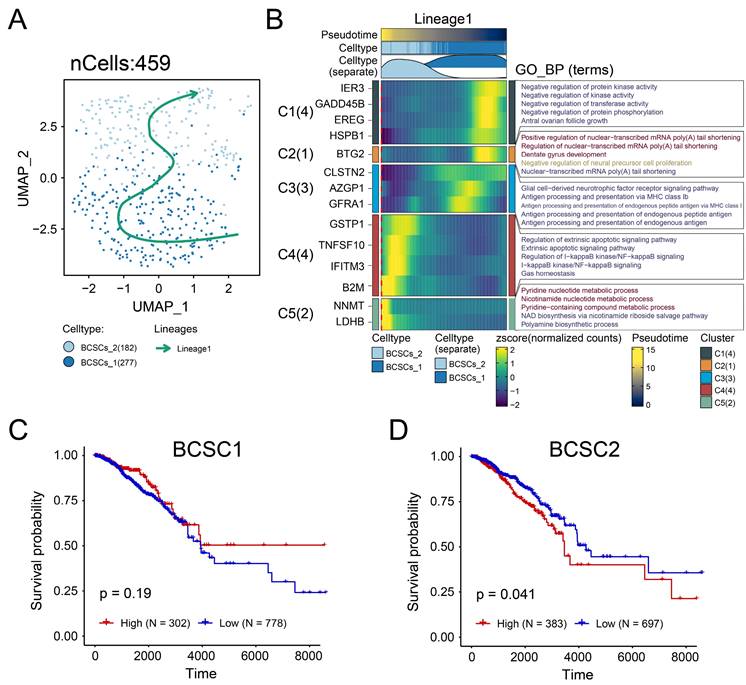
The enrichment of BCSCs-2 may reflect an increase in tumor malignancy. A-F The GSEA plot based on the signature gene sets reveals significant enrichment of different biological pathways in patients with high BCSCs-2 cell infiltration abundance. "Epithelial Mesenchymal Transition" (A), "PD-1 Signaling" (B), "Signaling By Interleukins" (NES: 2.03, Adjusted p-value: < 0.001, C), "Interleukin 2 Signaling" (D), "IL-6 JAK/STAT3 Signaling" (E), and "Interleukin 10 Signaling" (F).
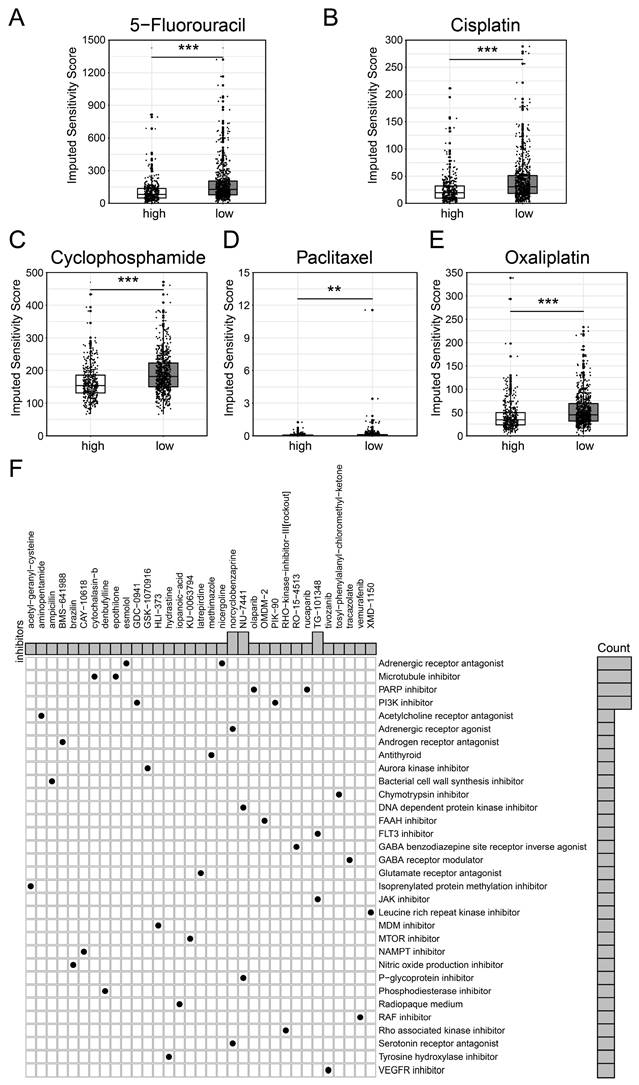
Drug Sensitivity Prediction Value of BCSCs-2 Cells
We first employed the 'oncopredict' package to evaluate the IC50 value of several chemotherapy drugs among BCSCs-2 groups. Specifically, patients with high infiltration abundance of BCSCs-2 may exhibit greater sensitivity to drugs such as 5-Fluorouracil (p < 0.001), Cisplatin (p < 0.001), Cyclophosphamide (p < 0.001), Paclitaxel (p < 0.01), and Oxaliplatin (p < 0.001) (Figure 6A-E). Most of these drugs are classic and reliable chemotherapy drugs for breast cancer[27, 28]. These findings provide new insights into the use of chemotherapy in breast cancer patients.
In addition, we used the CMAP database to screen potential therapeutic drugs targeting high BCSCs-2 group of patients (Supplementary Table S2). According to the mechanisms of various drugs, medications including norcyclobenzaprine, NU-7411, and TG-101348 had the potential to become specific therapeutic options for patients with high BCSCs-2 infiltration via the 'Adrenergic receptor agonist' pathway, the 'DNA-dependent protein kinase inhibitor' pathway, and the 'FLT3 inhibitor' pathway, respectively (Figure 6F). In conclusion, our study provides new insights and strategies for individualized precision treatment in some breast cancer patients.
Biological markers of BCSCs-2 were identified with gene co-expression modules. (A) Weighed gene co-expression network analysis was constructed among BCSCs. (B) The hdWGCNA dendrogram of 13 modules. (C) The distribution of characteristic genes of each module. (D) Dotplot was used to show the expression of characteristic genes in different modules. (E) Intersection of module genes and BCSCs differentially expressed genes.
Associates between the infiltration abundance of BSCSs_2 and somatic mutations. (A) The forest plot illustrates the differences in somatic single-nucleotide variants (SNVs) between patients with high and low BCSCs-2 cell infiltration. The OR > 1 indicates a higher SNV frequency in the high BCSCs-2 infiltration group, the OR < 1 indicates a higher SNV frequency in the low infiltration group, and the OR = 1 suggests similar SNV frequencies between the two groups. (B) Landscape of gene co-mutations with high infiltration of BCSCs-2. (C) Landscape of gene co-mutations with low infiltration of BCSCs-2.
Discussion
As far as we know, this study represents an innovative investigation of the unfavorable role of human BCSCs in tumor microenvironment of breast cancer by integration of multiple-scale data, including genomic data, expression profiles, and single-cell RNA profiles. Notably, we identified novel potential diagnostic biomarkers and therapy targets for BCSCs.
In general, BCSCs have been confirmed to play a critical role in tumor origin, development, recurrence, metastasis and therapy resistance in breast cancer[29, 30]. However, the constraints of previous sequencing technologies impede a comprehensive and nuanced characterization of BCSCs heterogeneity at the single-cell level within the intricate context of the tumor microenvironment. Fortunately, the advent of single-cell RNA sequencing and spatial transcriptomics has significantly advanced the ability to address these limitations. A large number of studies confirmed the malignant behavior and the heterogeneity of BCSCs. For instance, Nakayama et al.[31] found the two subtypes of BCSCs (HMGA1-high, CD44/MYC-high) existed in TNBC patients as well as TNBC xenograft models, indicating the heterogeneity and diversity of BCSCs by scRNA-seq and in vivo experiments. Ji et al.[32] revealed that BCSCs could promote immune escape in TNBC microenvironment through the upregulation of CTLA4-related signaling of CD8+ T cells.
Differential drug sensitivity analysis for patients with high and low BCSCs_2 cell infiltration. Boxplots (A-E) display the IC50 for standard chemotherapeutic agents, including 5-Fluorouracil (A), Cisplatin (B), Cyclophosphamide (C), Paclitaxel (D), and Oxaliplatin (E). Statistical significance is denoted by ** (p < 0.01) and *** (p < 0.001). (F) Dot plot of inhibitor functional enrichment illustrates the enrichment of inhibitors targeting diverse pathways based on CMAP analysis, with the x-axis representing specific inhibitors and the y-axis indicating their functional categories.
In addition, Li et al.[33] unveiled a subset of BCSCs with high expression of RAC2 and PTTG1 were significantly enriched in lymph mode metastasis, which might promote the tumor metastasis through modulation of immune system and activation of specific pathways. These studies highlight the interaction of BCSCs in the spatial heterogeneity and tumor microenvironment of breast cancer. Consistently, our study identified a subgroup of BCSCs (BCSCs-2) were associated with poor prognosis in breast cancer. Therefore, we focused on exploring the potential biological functions of BCSCs-2. The immune-related pathways including PD-1, IL-6/ JAK/STAT3, IL-10 signaling were significantly enriched in patients with high infiltration of BCSCs-2. These pathways have been confirmed to immune suppression[34-36]. The epithelial-mesenchymal translation was also highly upregulated in high infiltration group. Taken together, our findings revealed the BCSCs-2 may promote immune suppression and tumor metastasis in breast cancer microenvironment, which provides a theory basis on prognostic stratification and therapy targets for breast cancer.
As a high heterogeneous cells, BCSCs present a high plasticity[37]. Exploring the potential cell evolution trajectory of BCSCs can provide insight into the changes in their biological functions. We noticed the translational tendency from BCSCs-1 to BCSCs-2 with the dynamic enrichment of NF-kappaB signaling. Interestingly, NF-kappaB was proved to be involved in BCSC fate and expansion[38]. Also, some metabolic pathways (pyridine nucleotide, nicotinamide nucleotide, and polyamine) were gradually upregulated during the evolution, which highlighted the critical role of metabolic process for the evolution of BCSCs. Given the high risk of BCSCs-2, further identification of its biomarkers is warranted to guide therapy and risk stratification. We identified 16 candidate biomarkers (KMT2E, IFITM3, MAGED2, TM4FSF1, GSTP1, SRI, CD59, SLC39A6, LIMCH1, ATP1B1, DSP, SYNE2, RARRES3, TMC5, SLC40A1, and TM4SF18) for BCSCs-2. Although the efficiency of these biomarkers needs to be validated in clinic. Previous reports have demonstrated their potential. For instance, Singh et al.[39] developed a nanomedicine which could modulate GSTP1 to inhibit glycolysis in BCSCs, resulting in the overall tumor regression of TNBC. In a word, the above gene could be potential diagnostic biomarker and promising targets for breast cancer.
We then analyzed the association between somatic mutations and BCSCs-2 infiltration to better understand the underlying mechanisms of BCSCs-2 infiltration heterogeneity. It was noticed that high abundance of BCSC-2 were associated with somatic mutations of VPS13D, KMT2C, CHD4, FER1L6, FLNB, ZMTM3, while low abundance of BCSCs-2 was closely related to GATA3 mutations. Jiang et al.[40] reported GATA3 mutations were correlated with improved overall survival in breast cancer patients, and were mainly occur in patients with luminal-like breast cancer. Their conclusions support our findings that low-infiltrating BCSCs-2 was associated with a favorable prognosis. In addition, KMT2C/D are most frequently mutated histone methyltransferases and play a tumor-suppressive role in breast oncogenesis[41]. These findings have innovatively revealed the subtle relationship between somatic mutation and BCSCs infiltration heterogeneity, providing a new perspective and theoretical basis for further understanding the heterogeneity of BCSCs in the breast cancer microenvironment. Finally, we identified serval chemotherapy drugs and other potential drug for targeting BCSCs-2.
All in all, our study revealed the prognostic value, intrinsic lineage, potential biological processes, infiltration heterogeneity, personalized therapy strategy of BCSCs. However, the study also has some limitations. For instance, although we employed multi-scale data to explore the role of BCSCs, all the results were based on in silico analyses. The in vivo and in vitro experiments need to be performed in further study to validate our results. Furthermore, the sample size included in our study is limited. Therefore, we will collect more and different data sets to prove the generality of our conclusions. The bioinformatics is the first step of our study, and we meet the challenges in explaining the molecular mechanisms of our findings now. With a large number of high-quality clinical samples, sequencing profiles, and subsequent experiments, this issue will be addressed.
Abbreviations
TCGA: The Cancer Genome Atlas Program; GEO: Gene Expression Omnibus; TNBC: Triple-negative breast cancer; BCSCs: breast cancer stem cells; CSCs: Cancer stem cells; SNV: single nucleotide variant; QC: quality control; scRNA-seq: single-cell RNA sequencing; Cmap: Connectivity Map; UMAP: Uniform Manifold Approximation and Projection; tSNE: t-Distributed Neighbor Embedding; OS: overall survival.
Supplementary Material
Supplementary figure and tables.
Acknowledgements
We thank the personnel of the Gene Expression Omnibus (GEO) and The Cancer Genome Atlas Program (TCGA) databases for providing platforms and contributors for uploading their meaningful datasets.
Funding
This work was supported by National Natural Science Foundation of China (Grant Nos. 82304025, 82172835 and 82303857).
Author Contributions
GXW, XW, and YXL designed the study and collected research data; YT, SW, YXZ, and WBS were responsible for the interpretation of the results. YT, YXZ, and WBS analyzed data and drafted the manuscript; GXW, XW, and YXL provided the overall guidance. All authors read and approved the final Manuscript.
Availability of Data and Materials
The public datasets were obtained from TCGA (https://www.cancer.gov/tcga), GEO (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE180286).
Consent for publication
All authors have agreed to publish this manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024;74:12-49
2. Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73:17-48
3. Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-63
4. Giaquinto AN, Sung H, Newman LA, Freedman RA, Smith RA, Star J. et al. Breast cancer statistics 2024. CA Cancer J Clin. 2024;74:477-95
5. Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thurlimann B, Senn HJ. et al. Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736-47
6. Philchenkov A, Dubrovska A. Cancer Stem Cells as a Therapeutic Target: Current Clinical Development and Future Prospective. Stem Cells. 2024;42:173-99
7. Loh JJ, Ma S. Hallmarks of cancer stemness. Cell Stem Cell. 2024;31:617-39
8. Hassan KA, Wang L, Korkaya H, Chen G, Maillard I, Beer DG. et al. Notch pathway activity identifies cells with cancer stem cell-like properties and correlates with worse survival in lung adenocarcinoma. Clin Cancer Res. 2013;19:1972-80
9. Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003;100:3983-8
10. Dontu G, Al-Hajj M, Abdallah WM, Clarke MF, Wicha MS. Stem cells in normal breast development and breast cancer. Cell Prolif. 2003;36(Suppl 1):59-72
11. Charafe-Jauffret E, Ginestier C, Iovino F, Wicinski J, Cervera N, Finetti P. et al. Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Res. 2009;69:1302-13
12. Charafe-Jauffret E, Ginestier C, Iovino F, Tarpin C, Diebel M, Esterni B. et al. Aldehyde dehydrogenase 1-positive cancer stem cells mediate metastasis and poor clinical outcome in inflammatory breast cancer. Clin Cancer Res. 2010;16:45-55
13. Conley SJ, Baker TL, Burnett JP, Theisen RL, Lazarus D, Peters CG. et al. CRLX101, an investigational camptothecin-containing nanoparticle-drug conjugate, targets cancer stem cells and impedes resistance to antiangiogenic therapy in mouse models of breast cancer. Breast Cancer Res Treat. 2015;150:559-67
14. Conley SJ, Gheordunescu E, Kakarala P, Newman B, Korkaya H, Heath AN. et al. Antiangiogenic agents increase breast cancer stem cells via the generation of tumor hypoxia. Proc Natl Acad Sci U S A. 2012;109:2784-9
15. Luo M, Shang L, Brooks MD, Jiagge E, Zhu Y, Buschhaus JM. et al. Targeting Breast Cancer Stem Cell State Equilibrium through Modulation of Redox Signaling. Cell Metab. 2018;28:69-86 e6
16. Batlle E, Clevers H. Cancer stem cells revisited. Nat Med. 2017;23:1124-34
17. Wang Y, Song W, Li Y, Liu Z, Zhao K, Jia L. et al. Integrated analysis of tumor microenvironment features to establish a diagnostic model for papillary thyroid cancer using bulk and single-cell RNA sequencing technology. J Cancer Res Clin Oncol. 2023;149:16837-50
18. Wang G, Shi C, He L, Li Y, Song W, Chen Z. et al. Identification of the tumor metastasis-related tumor subgroups overexpressed NENF in triple-negative breast cancer by single-cell transcriptomics. Cancer Cell Int. 2024;24:319
19. McGinnis CS, Murrow LM, Gartner ZJ. DoubletFinder: Doublet Detection in Single-Cell RNA Sequencing Data Using Artificial Nearest Neighbors. Cell Syst. 2019;8:329-37 e4
20. Korsunsky I, Millard N, Fan J, Slowikowski K, Zhang F, Wei K. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat Methods. 2019;16:1289-96
21. Hafemeister C, Satija R. Normalization and variance stabilization of single-cell RNA-seq data using regularized negative binomial regression. Genome Biol. 2019;20:296
22. Hu C, Li T, Xu Y, Zhang X, Li F, Bai J. et al. CellMarker 2.0: an updated database of manually curated cell markers in human/mouse and web tools based on scRNA-seq data. Nucleic Acids Res. 2023;51:D870-D6
23. Newman AM, Steen CB, Liu CL, Gentles AJ, Chaudhuri AA, Scherer F. et al. Determining cell type abundance and expression from bulk tissues with digital cytometry. Nat Biotechnol. 2019;37:773-82
24. Wu T, Hu E, Xu S, Chen M, Guo P, Dai Z. et al. clusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation (Camb). 2021;2:100141
25. Mayakonda A, Lin DC, Assenov Y, Plass C, Koeffler HP. Maftools: efficient and comprehensive analysis of somatic variants in cancer. Genome Res. 2018;28:1747-56
26. Subramanian A, Narayan R, Corsello SM, Peck DD, Natoli TE, Lu X. et al. A Next Generation Connectivity Map: L1000 Platform and the First 1,000,000 Profiles. Cell. 2017;171:1437-52 e17
27. Tan WJT, Vlajkovic SM. Molecular Characteristics of Cisplatin-Induced Ototoxicity and Therapeutic Interventions. Int J Mol Sci. 2023;24:16545
28. Mafi A, Rezaee M, Hedayati N, Hogan SD, Reiter RJ, Aarabi MH. et al. Melatonin and 5-fluorouracil combination chemotherapy: opportunities and efficacy in cancer therapy. Cell Commun Signal. 2023;21:33
29. Lawson JC, Blatch GL, Edkins AL. Cancer stem cells in breast cancer and metastasis. Breast Cancer Res Treat. 2009;118:241-54
30. Badve S, Nakshatri H. Breast-cancer stem cells-beyond semantics. Lancet Oncol. 2012;13:e43-8
31. Nakayama J, Matsunaga H, Arikawa K, Yoda T, Hosokawa M, Takeyama H. et al. Identification of two cancer stem cell-like populations in triple-negative breast cancer xenografts. Dis Model Mech. 2022;15:dmm049538
32. Ji S, Yu H, Zhou D, Fan X, Duan Y, Tan Y. et al. Cancer stem cell-derived CHI3L1 activates the MAF/CTLA4 signaling pathway to promote immune escape in triple-negative breast cancer. J Transl Med. 2023;21:721
33. Li L, Liu J, Wang W, Fu Y, Deng Y, Li X. et al. Cancer stem cells promote lymph nodes metastasis of breast cancer by reprogramming tumor microenvironment. Transl Oncol. 2023;35:101733
34. Ibrahim SA, Gadalla R, El-Ghonaimy EA, Samir O, Mohamed HT, Hassan H. et al. Syndecan-1 is a novel molecular marker for triple negative inflammatory breast cancer and modulates the cancer stem cell phenotype via the IL-6/STAT3, Notch and EGFR signaling pathways. Mol Cancer. 2017;16:57
35. Dermani FK, Samadi P, Rahmani G, Kohlan AK, Najafi R. PD-1/PD-L1 immune checkpoint: Potential target for cancer therapy. J Cell Physiol. 2019;234:1313-25
36. Floudas A, Amu S, Fallon PG. New Insights into IL-10 Dependent and IL-10 Independent Mechanisms of Regulatory B Cell Immune Suppression. J Clin Immunol. 2016;36(Suppl 1):25-33
37. Walcher L, Kistenmacher AK, Suo H, Kitte R, Dluczek S, Strauss A. et al. Cancer Stem Cells-Origins and Biomarkers: Perspectives for Targeted Personalized Therapies. Front Immunol. 2020;11:1280
38. Velasco-Velazquez MA, Homsi N, De La Fuente M, Pestell RG. Breast cancer stem cells. Int J Biochem Cell Biol. 2012;44:573-7
39. Singh P, Sen K, Sa P, Khuntia A, Raghav SK, Swain RK. et al. Piperlongumine based nanomedicine impairs glycolytic metabolism in triple negative breast cancer stem cells through modulation of GAPDH & FBP1. Phytomedicine. 2024;123:155181
40. Jiang YZ, Yu KD, Zuo WJ, Peng WT, Shao ZM. GATA3 mutations define a unique subtype of luminal-like breast cancer with improved survival. Cancer. 2014;120:1329-37
41. Tinsley E, Bredin P, Toomey S, Hennessy BT, Furney SJ. KMT2C and KMT2D aberrations in breast cancer. Trends Cancer. 2024;10:519-30
Author contact
![]() Corresponding authors: Prof. Xin Wang, the First Department of Breast Cancer, Tianjin Medical University Cancer Institute and Hospital, Huan-Hu-Xi Road, He-Xi District, Tianjin, 300060, E-mail: wangxincom. Prof. Yingxi Li, Immunology Department, Key Laboratory of Immune Microenvironment and Disease (Ministry of Education), Tianjin Medical University, Qixiangtai Road 22, He-Ping District, Tianjin, 300070, E-mail: yingxiliedu.cn.
Corresponding authors: Prof. Xin Wang, the First Department of Breast Cancer, Tianjin Medical University Cancer Institute and Hospital, Huan-Hu-Xi Road, He-Xi District, Tianjin, 300060, E-mail: wangxincom. Prof. Yingxi Li, Immunology Department, Key Laboratory of Immune Microenvironment and Disease (Ministry of Education), Tianjin Medical University, Qixiangtai Road 22, He-Ping District, Tianjin, 300070, E-mail: yingxiliedu.cn.

 Global reach, higher impact
Global reach, higher impact